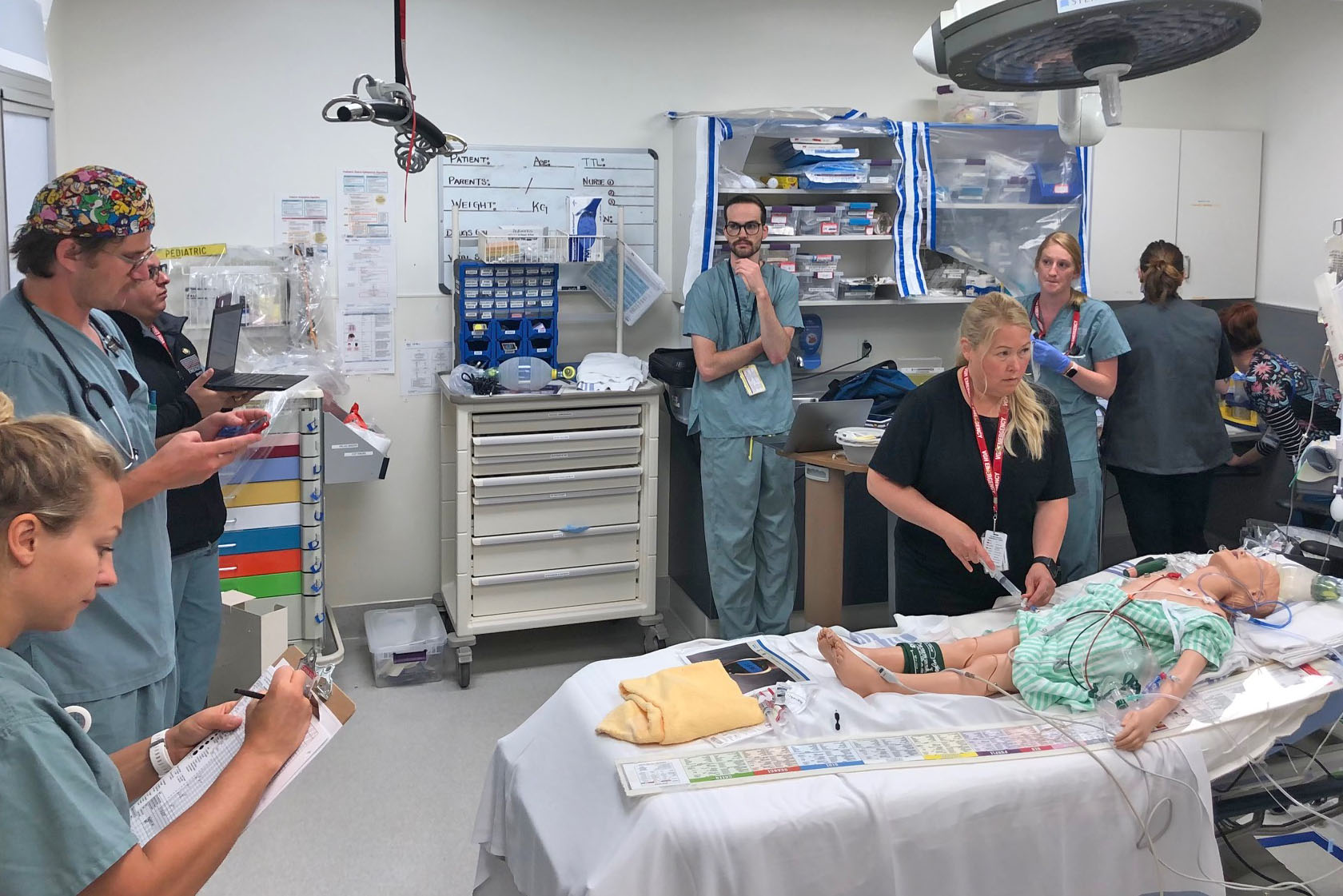
- Crisis reinforces the value of regularly simulating events
-
When the ‘heat dome’ descended recently onto British Columbia, many emergency departments were flooded with patients suffering from a dangerous condition known as hyperthermia.
Fortunately, Victoria-based Emergency Department (ED) physicians had run a hyperthermia scenario a year prior through its ED Simulation initiative, and identified important gaps in care that could be remediated. These included having ready access to cooled-IV fluids, body bags that could be filled with ice and water to further cool patients, and fans for misting.
Every month leaders from the 1,900-member Vancouver Physician Staff Authority (VPSA) and Vancouver Coastal Health (VCH) sit down to talk over mutual issues. They come to each meeting with an intentional focus that was agreed to by both groups and they rotate who chairs the meeting between VCH Interim President and CEO Vivian Eliopoulos and VPSA Managing Director Dr. York Hsiang. There is lots to talk about; both see physician wellness as a priority and they are also both invested in ensuring diversity, equity and inclusion among medical staff, and—for the past year—quickly communicating news regarding COVID-19.
VCH Physician Wellness Steering Committee
Since its start, VPSA has intentionally focused a large part of its work on wellness. In 2019, the health authority suggested combining forces to assess the level of burnout amongst physicians, to find its causes, and to develop collaborative solutions. The VCH Physician Wellness Steering Committee was formed with five health authority representatives and 12 VPSA members.
“We quickly realized we needed to understand what drives physician burnout and how that is different in every department,” said committee co-chair Dr. Zafrina Poonja. “We surveyed members in late 2020 and are now reviewing the data.”
Dr. Poonja credits the interdisciplinary composition of the committee with its ability to move the issues of physician wellness forward.
“We each bring a different perspective and it’s been important to have the support of VCH leadership. The health authority is invested in this issue and wants to do more so we can all be well; they’ve been very supportive. There are no quick fixes; there are issues within our system and within health care that are long standing. But if we can target micro interventions there could be a domino effect. It will take a lot of time and many grassroots initiatives, but my participation on this committee has made me hopeful.”

Communicating unexpected outcomes
Not all medical procedures go as intended and it is often left to physicians to deliver distressing news. It is therefore vital that physicians know how to communicate unanticipated results in a sensitive manner. VCH reached out to VPSA for help with this as it is a concern for both physicians and the health authority. VPSA funded a select group of skilled physicians to attend Communication of Unanticipated Outcomes in Healthcare training in fall 2020, thus developing an inhouse group of experts who will now teach the course to other physicians and health-care teams across the region.
“Partnering with VPSA on this project was paramount to ensuring physician engagement and collaboration,” said VCH Regional Director, Patient Experience Elizabeth Baron. “As we learn more about how to better include physicians as a part of our health-care teams and represent a cohesive approach to communicating with patients and families, we hope to see improved experiences for everyone. The impact of improved disclosure conversations—in addition to it being the right thing to do—has been shown to build trust in the organization, reduce fear of blame, decrease litigation against providers and the organization, and also shed light on organizational opportunities for improvement.”
“This project was a great example of recognizing a problem common to both physicians and the health authority, developing a response, and enacting solutions,” added Dr. Hsiang. “The educational leadership we’re creating will lead to improved communication skills that will ultimately benefit patients and their families.”
Later this year, the physician trainers will begin training their colleagues in communicating unanticipated medical outcomes.
Improving equity and inclusion in medical leadership
In January 2019, VPSA hosted an appreciative inquiry into meaningful leadership experiences and opportunities for women physicians. That work inspired the creation of the VCH Medical Staff Diversity, Equity and Inclusion (DEI) initiative. Eleven physician members sit on the committee along with four VCH medical leaders. The group’s work has earned praise from top VCH leadership including its board and interim president and it has changed the way VCH recruits medical leaders.
Over the past year, the committee held focus groups with women physicians about their experiences during the pandemic and it developed and launched a diversity survey to all VCH medical staff. It is about to begin physician Indigenous, Black and People of Colour focus groups and is planning an International Women’s Day event on gender equity in medicine.
“World events have made an impact on our work and there is broad interest in seeing DEI issues move forward at VCH,” commented committee member Dr. Joy Masuhara. “The health authority has started an organization-wide strategy and has valued getting physician input and feedback. We’ve taken a very co-creative approach and I feel that participating on the committee has helped foster better relationships between our groups. VCH is a large, complex organization and I have a better understanding now of the broader context for this work.”
“Without support from the VPSA committee members, the ability to influence a culture of change within the medical staff would be more challenging,” added VCH Manager of Physician Engagement Neli Remo. “The VPSA members have demonstrated courage and commitment to propel the DEI work to organization-wide levels and they continue to work tirelessly to advance and co-create an inclusive workplace.”
Welcoming new physicians to VCH
VPSA regularly hosts Meet and Greet events for onboarding physicians; its September 2020 event was held virtually via Zoom.
“Over 100 physicians joined our association in 2020 and we felt it was especially important to make them feel part of a community,” said Dr. Hsiang. “The pandemic has isolated us more than ever and we believe it is critical that we continue to take steps to break down silos between departments and divisions.”
VCH senior leaders attend these onboarding events and offer welcoming words. At the February 2019 event, Vivian Eliopoulos made these remarks:
“Our organization is our house and we need to have open and honest conversations about how we can make it the best possible place to be. There are discussions happening today that didn’t exist in a coordinated way before VPSA was formed and there’s a palpable energy encouraging us all to connect, collaborate and care. But [VCH leaders] can’t fix what we don’t know is broken. We want to hear from you so we can partner to make improvements.”
VPSA and VCH are now collaborating to survey newer staff to get a sense of what their pain points are in the onboarding process. The data will be used to craft solutions and improve their experience.
Communicating during a pandemic
There’s nothing like a common enemy to bring people closer together. A silver lining of COVID-19 has been the co-operation that it has brought about between groups like VCH and VPSA.
“We knew we would need to provide physicians with information about the virus that the hospital would be too busy to communicate,” said Dr. Vivian Yin. She and Dr. Sophia Park, who were both VPSA board members at the time, pulled information from the BCCDC and WHO websites and started a WhatsApp forum that touched on many COVID-19-related issues.
“VCH leaders were paying attention to WhatsApp and were impressed with how we were moderating it; they asked us to help them with physician communication. It was a timely request as we quickly outgrew WhatsApp and transitioned to the Slack platform that VCH medical staff continue to use to this day. VCH took over the platform and VPSA continues to provide support.”
The Slack channel has had a tremendous impact on physician engagement with specialists from various departments and divisions sharing knowledge rather than working in silos. Bridges have been built and leaders have emerged; it has also created a sense of community.
Early in the pandemic, VCH offered all-staff townhalls to update workers on the impact of COVID-19 on its sites. However, the information that physicians needed was different from that of, for example, nurses. VCH medical leaders Drs. Patty Daly and Chad Kim Sing understood that perspective and were amenable to suggestions for forums specifically targeted to medical staff. COVID-19 Virtual Medical Staff Forums debuted in March 2020 and have run regularly. Vancouver Acute also started offering a regular VA update.
Drs. Yin and Park were instrumental in the forums’ early days. They worked out the logistics and made sure physicians’ questions were gathered ahead of time.
“We stressed that all questions needed to be answered—even if it was only to acknowledge that they didn’t have an answer,” remembered Dr. Yin. “It’s increased the health authority’s transparency and it’s been new territory for VCH, which isn’t used to sharing so much information.”
“Medical staff communications have been well received during COVID-19 and these medical staff forums are a part of that,” said Dr. Kim Sing. “These efforts have led to deeper and more meaningful engagement and we’ve been able to continually improve our dialogue and communication with and between our medical staff colleagues.”
There is interest in continuing the medical staff forums in the post-pandemic world. The format and frequency may change but, in Dr. Yin’s eyes, COVID-19 has opened the VCH leadership’s mindset to getting more physician input.
Vivian Eliopoulos agrees. “One of the positive things around the pandemic is the networking across the organization that has occurred and it’s something we certainly want to continue,” she said. “My hope is that our forums don’t stop. Eventually we’ll move away from talking about COVID and vaccine planning into other areas of interest for our physicians.”

 These are challenging times in BC, and staying positive is more important than ever.
These are challenging times in BC, and staying positive is more important than ever.
 Martin explains that traditional cleansing ceremonies have been used by her ancestors for generations and continue today. “
Martin explains that traditional cleansing ceremonies have been used by her ancestors for generations and continue today. “ “A First Nations Cultural Worker came to the hospital to do a cleansing ceremony for some patients,” he says. “We didn’t see any of those patients for more than a year after. When I would see them in the community, I could see they were doing better. That is hard to ignore."
“A First Nations Cultural Worker came to the hospital to do a cleansing ceremony for some patients,” he says. “We didn’t see any of those patients for more than a year after. When I would see them in the community, I could see they were doing better. That is hard to ignore." Chris Seitcher has worked in the helping field for many years, including as a care aid with Island Health, and for elders in the Tla-o-qui-aht
Chris Seitcher has worked in the helping field for many years, including as a care aid with Island Health, and for elders in the Tla-o-qui-aht
 Over time, the aim of those involved is to introduce traditional healing practices more widely with health care professionals, ambulance crews, firefighters, the coast guard, and police officers—all of whom are exposed to emotional and physical trauma—and to create stronger cultural connections among patients, health care, and emergency professionals.
Over time, the aim of those involved is to introduce traditional healing practices more widely with health care professionals, ambulance crews, firefighters, the coast guard, and police officers—all of whom are exposed to emotional and physical trauma—and to create stronger cultural connections among patients, health care, and emergency professionals.