- Provincial

Supporting physician health & wellness through engagement and collaboration
Read More Read LessFacility Engagement is supporting physician health and wellness through collaborative opportunities to engage with health authorities and others to participate in workgroup, organizational and system improvements.

Rates of physician burnout and moral distress were rising before the COVID-19 pandemic.
They continue to rise due to increasing demands on physician time and resources in a complex and, at times, constrained health care system that involves heavy workloads and clinical practice requirements, inefficient system processes, and evolving technology.
Physician burnout and stress has been associated with impacts to patient care quality and health care system capacity with decreased productivity and turnover.

Emotional exhaustion, devastating mental health and physical issues, inability to concentrate are a few impacts of burnout reported through the 2019 Doctors of BC Physician Burdens survey.
Physician members reported:
- Unmanageable workloads and loss of work-life balance
- Decreased job satisfaction and joy in practice
- Disengagement, unable to influence change
- Reduced work hours or services, changing specialties, leaving the profession
Doctors of BC – Physician Burdens Member Feedback


Individual approaches to improve physician health and wellness are important. But burnout is often a result of challenges experienced in the physician work environment at the local work group and/or organizational level.
The Specialist Services Committee (SSC) Facility Engagement Initiative recommends that medical staff associations (MSAs) focus engagement funding and activities for physician wellness primarily in areas of work group-level/ organizational-level improvements or in combination with individual level strategies.
Physician wellness advocates suggest that about 20% of burnout is impacted by individuals while as much as 80% is impacted by the practice environment / organization.* They also recommend to maximize physician well-being, both individual and organizational/system level strategies are needed (West, Dyrbye, Erwin, & Shanafelt, 2016).
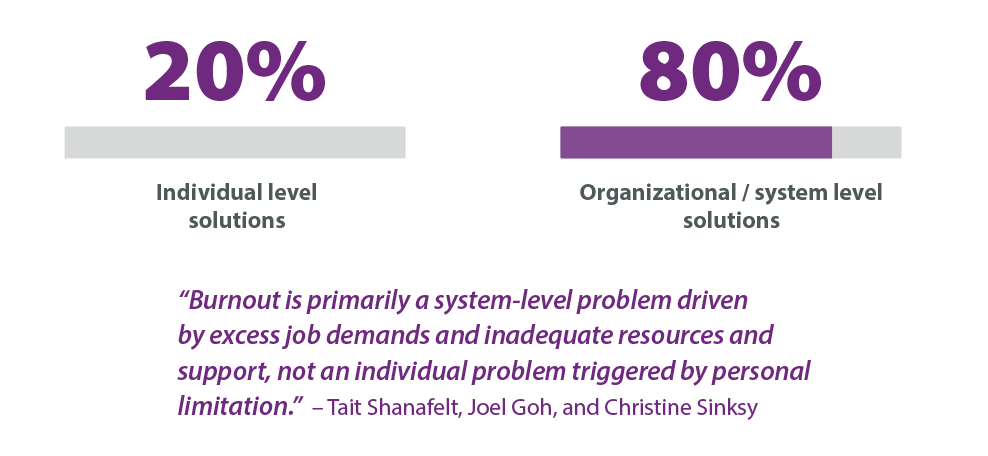
*Suggested areas of focus: Dr. Tait Shanafelt, a leading international expert on wellness; the Canadian Medical Association; Canadian Medical Protective Association. See below for more references.

In BC, physicians have opportunities to address some of the workplace and organizational-level issues that contribute to stress and burnout through the Joint Collaborative Committees (JCCs), which includes SSC Facility Engagement. Physicians can:
- Join and engage in collaborative entities such as MSAs, divisions, networks, communities of practice, and others and have a united voice no matter where they practice.
- Create strong relationships and formal collaborative processes with health authorities, physician colleagues and others to work together on problems and improvements.
- Tailor solutions to local challenges, and/or work on common challenges at the organizational, regional and/or provincial levels, such as care coordination, patient transport, electronic health records, and recruitment and retention.
- Lead a spectrum of improvement initiatives to energize and stimulate better practice environments.
- Connect with other physicians to build community, collegiality, self care and peer support, recognize accomplishments, reduce isolation, and support each other in the care for patients.
READ MORE: BC's Joint Collaborative Committees


The Joint Collaborative Committees have also partnered with the Physician Health Program of BC to start developing and supporting provincial resources for individual physician health, including:
- Networks of trained physicians offering their colleagues one-to-one peer support.
- Services to match physicians with their own family physician to support their primary care needs.
- Core cognitive behavioural skills training for physicians to support their health and wellness.
At the same time, Doctors of BC continues to enhance and develop programs to meet the current and future individual wellness needs of its members. Read about supports here >

References and related links:
- Shanafelt, T.D. (2021). Tait Shanafelt, MD, on addressing physician burnout. AMA.
- West, C. P., Dyrbye, L. N., Erwin, P. J., & Shanafelt, T. D. (2016). Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. The Lancet, 388(10057), 2272-2281.
- Mayo Clinic Strategies to Reduce Burnout e-book: 12 Actions to Create the Ideal Workplace (Swensen and Shanafelt). Borrow an e-book from the College of Physicians and Surgeons of BC (will need login).
- Canadian Medical Association: Addressing burnout at a systems level
- CMPA Canadian Medical Protective Organization (CMPA): Guide to healthier physicians: An investment in safe medical care.
Facility Engagement in Action: 2016-2020
Read More Read LessRead about how Facility Engagement is making a difference in BC! This publication brings together just a few examples of the many successful Facility Engagement activities that are transforming engagement in BC >

Facility Engagement: What is changing?
Read More Read LessA lot has changed in the four years since the Specialist Services Committee launched Facility Engagement across BC to strengthen meaningful physician involvement in health authority decision-making.
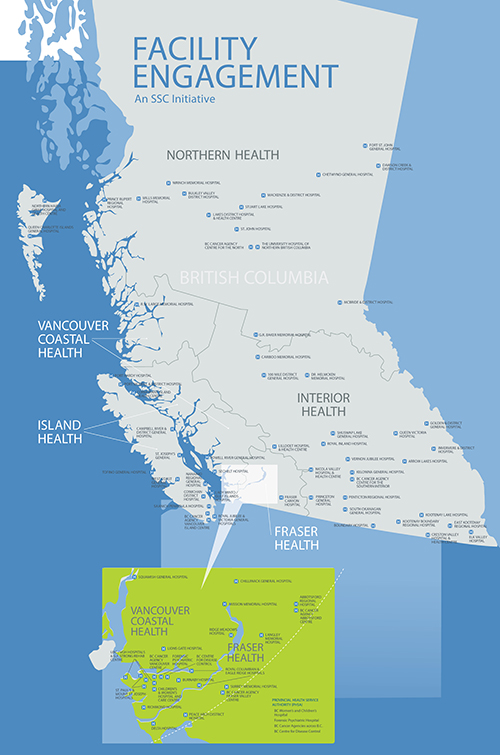
- Across BC’s acute care facilities and programs, 72 Medical Staff Associations (MSAs) in 6 health authorities have galvanized more than 4,300 physicians to participate in 2600+ Facility Engagement activities. (Updated to February 2020).
- A combination of new structures, funding, physician leadership, and administrative supports are enabling MSAs and their physician members to improve engagement and teamwork among colleagues and with health authorities, in ways that were not possible in the past.
- The UBC evaluation of Facility Engagement to March 2019 found that medical staff and health authority leaders think that participation in the initiative is worthwhile.
With all of this activity – and a lot of hard work – a sense of optimism is fueling a growing culture of engagement across BC, with renewed teamwork and positive experiences reported by many of those involved.
Big themes: Foundation for change
“This is an exercise in relationships – setting a foundation that allows us to grow as an organization, as people, as a team, as partners in care.” – Dr. Harsh Hundal, Executive Medical Director Physician Engagement & Resource Planning, Interior Health
Physician-to-physician communication and relationships are improving as a key step for MSAs to build a strong foundation for engagement and a medical staff voice. Physicians are connecting and meeting across sites and regions – for the first time ever in some cases – to get to know and support each other, discuss priorities and work on projects that strengthen their hospital, patient care, and personal well-being.
Communication with health authorities is improving. At many sites, MSA working groups and physician members are regularly meeting and establishing collaborative processes with health authority administrators and leaders to discuss respective priorities, and to work on projects together.
Physician wellness has also surfaced as a priority, with MSAs across BC initiating activities that aim to reduce the risk of burnout and support physicians to provide patient care in a healthier way. Some MSAs are now starting to elevate these efforts to an organizational, regional and system level to look at potential improvements that can reduce the risk of burnout. (Doctors of BC is further working on this priority through the Physician Burdens engagement and policy development process.)
With the new 2019 Physician Master Agreement, Facility Engagement is also officially supporting medical staff engagement in the implementation of electronic health records, starting with Lower Mainland hospitals that are adopting the Cerner system.
Moving Forward
There is more work to be done to achieve sustained change, and further evaluation of the Facility Engagement Initiative will to measure its ongoing impact. Meanwhile, both physicians and health authority partners from many parts of the province report they are making headway to build trust and to make decisions together that impact their hospitals, programs, work culture and patient services. Stay tuned as this great work continues to unfold!
Read examples and successes > www.facilityengagement.ca/stories

Physician spaces: one step to avoid burnout
Read More Read LessOne the key priorities for MSAs in Facility Engagement is to improve relationships among doctors. At larger sites, many physicians don't know who their colleagues are and have not connected for years in some cases.
Having a collegial community and spaces where physicians can get to know each other, share conversations and have room to breathe not only helps doctors deal with the intense stresses of hospital work and potential burnout, it also helps with patient care.
When physicians know who's who, it is easier to ask a colleague for a consult or advice when having a patient care challenge.
In Facility Engagement, MSAs have planned a number of activities that enable physicians to connect and get to know each other, which includes carving out dedicated, quiet space for them to have a conversation, make a phone call, or just get away from the hubbub of the unit to gather their thoughts.
MSAs in BC are not alone in recognizing the value of having a physician lounge.
Facility Engagement: Relationships drive change
Read More Read Less- The Facility Engagement Initiative continues to gain momentum with 69 hospital-based physician groups now organized and leading more than 500 projects across BC. So what is energizing this activity?
Mainly, it’s relationships. My father, who was an obstetrician, worked at the tertiary care teaching hospital in Edmonton. He used to say he would not infrequently see Dr Snell—the CEO of the hospital at the time—in the hallway. If there was an issue to discuss, the two of them would just talk about it.
Today, doctors may never see the CEO or other senior executives. There’s not a one-on-one relationship anymore, for a variety of reasons. The pressure on resources, staff, and the whole system is so much greater. We can’t expect to be able to stop Dr Snell in the hallway and talk to him about our issues.
As a result, for the past few decades, physicians have felt that they’ve lost their voice. They are not always asked about critical decisions that impact patients. When concerns arise, often physicians don’t know whom to contact in the health authority structure. After asking the same question over and over, nothing changes, and they stop engaging. I experienced this personally, and have heard it consistently in surveys and interviews with hospital-based doctors.
That’s why we introduced Facility Engagement. It specifically aims to remove this barrier that doctors feel so discouraged about. It encourages health authorities and doctors to talk to each other and build relationships, and gives physicians time and more opportunity to influence decisions affecting their workplace and patient care.
We’re optimistic that Facility Engagement is creating an environment for change, but it will continue to take effort on the part of physicians and health authorities.
How will we know if it is working? When doctors are able to prioritize the issues most important to them and discuss them with the health authority, and say, “We’re organized now. We’d like to be involved.” And when the health authority comes to physicians to ask for input about their 10-year plan or important clinical decisions before they make them, and says, “We should talk to these doctors. They know what they’re doing.”
That doesn’t mean that every doctor will get what they want. But if physicians have a chance to weigh in and be involved, we will make some progress.
We also realize that doctors need to do a better job of talking to each other about their issues. Through this initiative they are doing more of that, and I hear they are enjoying it.
In my previous role as head of surgery, my colleagues and I agreed to reallocate some OR time from one surgical service to another, based on information that we discussed openly. The group that gave up the OR time realized it was not right that cancer patients from the other service were waiting longer than their own patients who had less-serious problems.
Supported by good information, we simply talked, and our patients benefited, which, in the end, is the whole point.
Facility Engagement is sponsored by the Specialist Services Committee, one of four committees representing a partnership of Doctors of BC and the BC Government. Read more about Facility Engagement progress at www.facilityengagement.ca.
—Sam Bugis, MD
Executive Director, Physician and External Affairs, Doctors of BC(originally published in the BC Medical Journal, April 2018)
- Fraser Health

Maternity service wait-times drop from 3 months to 3 days
Read More Read LessDr Charlene Lui, a family physician at the Burnaby Maternity Clinic, led a project to reduce clinic referral wait-times from up to 90 days to just a few days through an SSC Physician Quality Improvement. Read the story here>

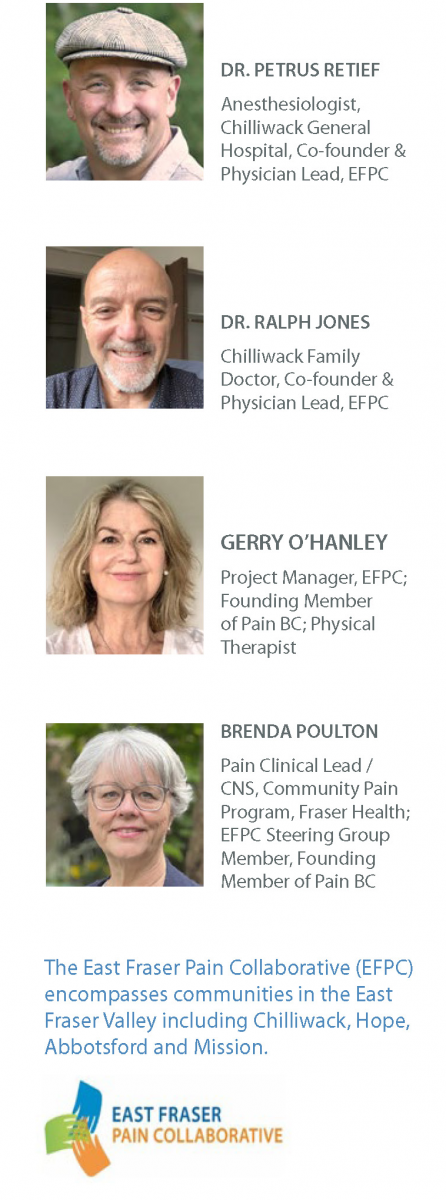
East Fraser Pain Collaborative: Engagement to tackle chronic pain
Read More Read LessA group of health care innovators in the Eastern Fraser Valley (Chilliwack, Hope, Abbotsford and Mission) is on a mission to improve the lives of people who experience chronic pain. The East Fraser Pain Collaborative (EFPC) is a physician-initiated, region-wide engagement effort that is creating a seamless, coordinated, easily navigable system of care for patients and providers to prevent and manage chronic pain.
 Chronic pain is often an undertreated condition that causes havoc in people’s lives. Patients suffer and feel judged; they are socially isolated and can’t fully work. They are four times more likely to have depression and anxiety; and two times more likely to be at risk for suicide and to have concurrent substance use disorder.
Chronic pain is often an undertreated condition that causes havoc in people’s lives. Patients suffer and feel judged; they are socially isolated and can’t fully work. They are four times more likely to have depression and anxiety; and two times more likely to be at risk for suicide and to have concurrent substance use disorder.Not surprisingly, there is a direct relationship between chronic pain and the opioid crisis. In BC, among people who died of illicit drug overdoses in 2018/19, 45% had reached out to health care services with pain issues.
Chronic pain is not just a symptom; it is a disease. The longer pain exists, the more permanent the change to the nervous system, and the more difficult it becomes to treat.
Timely, individualized treatment is needed; but patients and doctors alike feel helpless because often there is no system in place through which to access consistent resources, services and knowledgeable pain practitioners. Often, patients end up in the emergency room because they have nowhere else to go.
In the Eastern Fraser Valley, 20% of the population have chronic pain issues at any given time – that’s over 65,000 patients, with about 18,000 experiencing a major impact on the quality of their lives.
Patients and doctors alike feel lost to effectively manage and treat pain
The genesis of the EFPC came from two physicians, Dr Petrus Retief, a Chilliwack Hospital Anaesthesiologist and Dr Ralph Jones, a Chilliwack Family Physician. Dr. Retief started a pain service in Chilliwack in 2011 as an Anesthetist providing interventional pain management treatments.
“The more I got involved, the more I realized what an undertreated and underappreciated part of the patient community it was,” he said. “And more I tried to motivate for us to be able to manage these people, the more I ran into brick walls.”
Dr. Jones had his own experiences in his family practice. “Patients feel lost and so do we [as doctors],” he said. “We get so far and hit walls when it comes to resources or acquiring timely help.” He noted that patients can wait year to 18 months for specialist service tertiary services – only to return to him much the same, because next steps are not built into the system.
“There are no next steps, no way to take any learnings forward. There’s no medical system, no social system, no mental health help.”
Wanting to do better, the pair approached the Chilliwack Medical Staff Association (MSA) in 2019 for Specialist Services Committee Facility Engagement funding.
Dr Retief, who had been working on a pain clinic for a decade without an official budget, said the funding was ‘utopia’ and just breakthrough they needed to make the right links and alliances, and engage professional project support, Gerry O’Hanley, to navigate the work. Brenda Poulton, the Fraser Health community pain program clinical lead, was also engaged to support the initiative.
The MSA showed unwavering support and commitment from the beginning, with further vital support, guidance and sponsorship provided by Fraser Health and its Executive Director for the Chilliwack area, Petra Pardy, who also sits on the MSA.
Engagement of the health care community: foundation for success
Widespread engagement would pave the way to success. “They created this East Fraser Pain Collaborative which was absolutely amazing because they had a vision about the importance of education, collaboration, bringing people together, partnership and they developed a mission,” said Gerry O’Hanley. “They were going to bring about an integrated system of providers working together.”
Given the complexity of chronic pain, the group recognized that they would need to bring together all providers involved: no one could be left out.
Dr Retief said, “Our first objective was to identify pain champions in our community, and it just grew from there.”
To get started, they identified a Strategic Planning Team to lead the work ongoing. Membership includes a patient with lived experience, and ten core stakeholders representing specialist and family physicians/Division of Family Practice, Fraser Health managers and staff, nurses and a physiotherapist. “We brought them together and said, ‘this is a network, we collectively own this,’” said O’Hanley.
Identifying the problems
Together they created a charter, and of key importance, aligned it with the Fraser Health Regional Chronic Pain Prevention and Management Strategy and other pain strategies and work. They embarked on a discovery process which involved talking to patients and providers, and identified five areas that cause chronic pain to be undertreated and mismanaged:
- A lack of awareness about what chronic pain is, from both patient and provider perspective
- A lack of communication and collaboration between treating physicians and providers
- A lack of knowledge and skills among providers
- A lack of governance and ownership for chronic pain
- A lack of resources including services and budget
For maximum engagement, they created a broader reference a group to explore solutions, which has since grown to about 100 members. It includes primary care physicians, divisions, allied and community health providers, Fraser Health clinical staff and health care managers, chronic disease management leaders, as well as clinics in Abbotsford, Mission and Hope.
Identifying solutions
Through engagement and input, solutions were identified that are grouped into four pillars for change, with Working Groups for each.
- Patient education and public awareness: Education about the science and impacts of pain, a Patient Roadmap for self-care resources, and public awareness campaign.
- Provider education: Skills and knowledge-building; a Provider Education Roadmap; connections to local community resources; and a database of resources.
- Service provision: A transitional pain service (Anesthesia) to manage pain and optimize recovery before and after surgery; services for marginalized and unattached patients; East Fraser Valley Pain Hub services expansion; central intake; and a rapid access clinic.
- Outcome evaluation: Inputs, outputs, and metrics to measure progress, and modify the initiative as needed.
Read more about these solutions>
Patient education and awareness is one of the highlights. “Patients do much better if they can have some understanding of the complexity and how we understand pain, the changes that happen in the brain and the nervous system in chronic pain,” said Brenda Poulton.Additionally, she noted that having connections to self-management programs with Allied Health Care providers and nurses can make a big difference to a patient's level of pain, their sleep, mental health and mobility.
Moving forward
The group continues to build out the pillars of change, enabled by the engagement and passion of the champions, effective communication channels, and enhanced cooperation and collaboration with patients, local allies, the MSA and divisions, and regional and provincial stakeholders – including Fraser Health, the Ministry of Health, PainBC, Shared Care, and the First Nations Health Authority.
The continued engagement has put the initiative on a solid path towards achieving its ideal state, which is a multi-layered, interdisciplinary management platform that provides biopsychosocial treatment plans and maximizes information technology for central triaging, coordination, and information sharing.
“It will be absolutely awesome,” said Dr. Retief of the unfolding future state. “The moment I see a complicated patient, and there’s no way I can manage this patient on my own, I can say, “Okay, this is how you can get started on that pathway. The patient will immediately feel they are part of something. Somebody is taking care of them and they are linked into something bigger.”
“It’s our flagship program and we’d be very happy to help people to spread it. You don’t need reinvent the wheel every time you set up a program like this in any community in BC.” - Dr. Ralph JonesPhysician engagement in this initiative is funded by Facility Engagement, an initiative of the Specialist Services Committee.
Working together: The East Fraser Pain Collaborative Strategic Planning Team
Dr. Petrus Retief, Anaesthesia CGH – Chair; Dr. Ralph Jones – FP specializing in MHSU and Frail Elder Care with an interest in Chronic Pain and Addiction; Brenda Poulton, FH Clinical Lead/Community Pain Program; Dr. Cameron Ross, FP in Chilliwack and the local Chronic Pain representative in the Chilliwack FP Division and SC Initiatives; Dr. Aman Haji, Abbotsford Division of Family Practice – interest in Chronic Pain Management and Addiction Medicine; Dr. Jeff Van Huizen, Abbotsford Division of Family Practice, Petra Pardy, Executive Director, Chilliwack, Hope and Agassiz Health Services, CGH and FC Hospitals; Dwayne Patmore, Patient Representative; Roly Fletcher, PT, MSc, UBC Faculty of Medicine, Department of Physical Therapy; Cristina Rouiller, Project Manager, Mission Division of FP, Dr. Peter Frew, Mission, Division of Family Practice; Dr. Aaron MacInnes, Anaesthesia SMH and JPOCSC, Division of Pain Medicine, FH; Dr. Aseem Grover, FP in Hope specializing in Chronic Pain Management and Addiction Medicine; Dr. Cat Mattheus, Anaesthesia ARHCC; Tracey Arsenault, Project Manager, Chilliwack Division of Family Practice; Kiefer McNaughton, Heritage Chiropractic, Chilliwack, and Gerry O’Hanley, EFPC Project Manager. Corresponding: Daphne McRae, ED Chilliwack Division of FP; Shona Brown, ED Mission Division of FP; Monica Mamut, ED Abbotsford Division of FP, Gene Patterson, Project Manager, Abbotsford Division of FP; and Meghann Coughlan, Communications and Outreach Lead, Abbotsford Division of FP.

Maintaining physician wellness during Covid-19 and beyond
Read More Read LessDoctors are working hard to provide the best care for their patients during the COVID-19 pandemic. These unprecedented times add stress and anxiety to physicians and frontline workers who may already feel burned out.
“I think most of us are just feeling tired,” shares Dr Laura Kelly, department head of Emergency Medicine at Ridge Meadows Hospital. “I'm seeing a fair amount of covert fatigue not just in doctors, but in all health care workers. A lot of people are exhausted.”
Dr Kelly and her colleague Dr Connie Ruffo, a White Rock hospitalist, recognized that doctors were potentially facing their own health crisis.
It’s why the doctors spearheaded swift efforts to prioritize the well-being of themselves and their colleagues through the Fraser Health Physician Wellness Committee, which is co-chaired by Drs Kelly and Ruffo.
As part of its work, the committee declared November as Physician Wellness Month in Fraser Health to keep health and well-being top of mind for all medical staff.
Also, the third annual Physician Wellness Forum held in November pivoted to accommodate pandemic restrictions, changing from an in-person event to a series of virtual workshops throughout the month.
Dr Kelly observed that the virtual sessions tried to accommodate both community- and hospital-based physician schedules, making it easier for doctors and medical staff to pop-in to the two-hour sessions at the end of workdays.
More than 100 doctors and medical staff joined weekly workshops to reflect on how to strengthen their personal wellbeing and of their colleagues. Topics included sources of wellness support, including community wellness teams, energy management, peer support, and compassionate leadership.
The forum is sponsored by the Fraser Health Authority and regional medical staff associations and divisions of family practice, and received funding for the first two years from Facility Engagement, an initiative of the Specialist Services Committee.
“The work we are doing for physician wellbeing highlights how vital Facility Engagement is in supporting physician partnerships with health authorities to nurture system change.”
Collaborating for cultural change
Dr Kelly notes that a doctor’s wellness is more than just caring for personal health through exercise, nutrition, or yoga. It’s also about connecting with peers to support one another. It is also about doctors engaging with the health care system to create changes that reduce the risk of burnout by improving efficiency and effectively delivering patient care.
For more than 15 years, Drs Kelly and Ruffo have been championing a shift in the culture of wellness at the grassroot level. They have been working with their peers, along with local and regional partners including MSAs, divisions, and Fraser Health. Together, these groups are fostering more peer-to-peer conversations, modelling compassionate leadership, reducing stigmas, and creating safe spaces.
In recent years, Drs Kelly and Ruffo have been working with colleagues and health care partners to develop a regional wellness strategy, visions and mission –a first of its kind in BC.
Recalling how she and Dr Ruffo got started, Dr Kelly says they modelled peer support by reaching out to colleagues who were distressed, sad or acting out, and fostered collegiality by hosting wellness activities where there were conversations about suicide, addiction, burnout, and how to look after a patient who's also a doctor.
Dr Kelly’s advice to other doctors is to do for themself and their colleagues as they would for their patients.
“It's just a matter of saying ‘I'm here. How are you? or I'm noticing this; how can I help?’”
Dr Kelly says that simply taking the time to truly listen and hear a colleague is what peer support is about.
“If you have people in each community that are modelling peer support, then they are seen as advocates for their colleagues,” says Dr Kelly. “And then we have real movement in the culture shift that we're trying to make –that physicians are valued and supported.”


Physicians Advocating for Wellness: Thinking Bigger
Read More Read LessFraser Health’s regional Medical Staff Wellness Committee has been working with physician health champions from its 12 hospitals and 10 divisions, as well as health authority leadership, to sow the seeds for a regional Physician Health Program.
Dr. Connie Ruffo is a physician health champion of Peace Arch Hospita and Fraser Health's Physician Wellness program. She has been involved in physician health efforts for more than a decade. She notes that “physician health” includes not only physical, mental and social well-being but the element of professional fulfillment which gives happiness and meaning in work.
She sees three influences on our well-being as doctors:
- How we care for ourselves. “Basic health practices –what we eat, how much we exercise, sleep, connect with family and friends. This, combined with resilience skills such as boundary setting, mindfulness, and energy management eases the distress of burnout; but alone won’t prevent it. This element is very much under our control.”
- How we care for our colleagues. “This involves connecting and reaching out to support one another. Humans are wired to connect. We listen to our patient’s stories everyday. It is also important for doctors to share their stories. Sharing and connecting means feeling safe enough to be vulnerable. Doctors understand doctors. This gets to culture, and changing how we communicate and interact with each other.”
- How we engage in changing the system. “Once physicians become better connected, then it is easier to build healthy teams. Whether in the OR, the ER, hospitalists or other specialities, or divisions of family practice, we are all part of the system. Physicians have key skills and insights, and a professional responsibility to be leaders, advocates, educators and innovators. Together we really can influence system change. We can educate administrators and executive decision-makers, initiate and lead patient quality improvements and projects, and provide input on system proposals or decisions that will impact how we do our work to care for patients, and our well-being. Facility Engagement funds are an amazing opportunity to do this. We can choose where to direct our energy to make system changes to areas that burn us out.”
Dr. Ruffo refers to a landmark Mayo Clinic study which revealed that organizational-driven efforts which address workplace drivers of burnout (e.g. work flow, efficiency, technology) and provide opportunity for self-care, reduce burnout and promote engagement, can have an even greater effect than physician-driven wellness events.
"There are many organizational interventions that require small investments, yet have a very large impact. Involvement by physician leaders, and administrator attention to these factors were key to its success," she says. Examples include supporting teamwork, training compassionate leaders and enhancing EMR efficiency.
“This is a very exciting time for those of us that have been involved in physician health over the years. There is an explosive amount of research being done around the world. There are new tools for measuring well being in physicians. And, province-wide there is a phenomenal grass-roots movement occurring among doctors, who are declaring their need for vigorous community- based wellness programs, which are supported and acknowledged both regionally and provincially.”

FRASER HEALTH SHARES ITS SUMMARY OF FINDINGS
Fraser Health’s Medical Staff Wellness Committee wish to share the findings of their experiential workshop with other MSAs, divisions and health authorities,with the view that taking the priority of physician well-bring to an organizational/ system level will help to raise awareness and stimulate action around this urgent issue across the province. Some of the themes and directions they want to start exploring are here.
Acknowledgements: The event developed for the FH Medical Staff Wellness Committee would not have been possible without the work of Dr. Elizabeth Froese and Dr. Laura Kelly. Also, the support of Dr. Dayan Muthayan, Physician Partnerships, Fraser Health and Facility Engagement Director Cindy Myles were instrumental in its realization.
Related links
- Physician Health at the individual and system level: Canadian Medical Association policy > (Go to abstract and download PDF)
- Mayo Clinic: Organizational Strategies to tackle physician burnout > (Go to abstract and download PDF)

Surrey Memorial Hospital to start emergency physician residency program
Read More Read Less- Dr. Sally Barrio, an emergency physician, has helped champion new ER physician training at the Surrey Hospital, reportedly the busiest ER in Canada with over 450 patients a day. It has been a dream for a some time at Surrey Memorial. READ MORE >

Burnaby Hospital Engagement Efforts Pay Off
Read More Read LessBurnaby Hospital physicians have been working to leverage the Facility Engagement opportunity to improve patient care and their workplace, and to build relationships among physicians and with the hospital administration. Their efforts are paying off. The following are a few examples of the great work underway that is leading to positive changes for the hospital.
Education Forum: Community Physicians Meet Specialist Services
Project Lead: Dr. Chris Bozek
Burnaby community physicians had little information about the existing speciality services and resources that Burnaby Hospital is able to provide to their patients. Furthermore, some physicians expressed lack of awareness about how to successfully refer their patients to the speciality clinics such as the orthopedics or neurology clinics at Burnaby Hospital.
So they set out to increase the knowledge and awareness of the hospital's specialty services, and establish effective communication between all physicians to improve patients’ experience in receiving timely and appropriate care. Their goal was to ensure patients have access to the right treatment to the right patient at the right time - every time.
Changes made: A steering committee was formed with the Burnaby Hospital project champion and Executive Director, and the Division of Family Practice, to discuss potential topics of discussion and best way(s) to present information. Three meetings were held, and a number of different topics were generated.
Project Outcomes: 3 education forum events have been held with over 30 participants attending:
May 3, 2018 – Ortho 101 - Review of the central intake for Orthopedics
- Overview of hip arthroscopy and minimally invasive hip replacement
-10 myths around Orthopedics
- Roundtable discussionOctober 18, 2018 – Neurology - Migranes/Headaches
- Multiple Sclerosis
- Seizures & Epilepsy
- Neuromuscular Disorders
- Roundtable discussion - Improving Access to Neurology Consults in BurnabyApril 10, 2019 – Chronic Pain Management - Procedures for pain management
- Medical management of chronic pain
- Pain management programs
- Roundtable discussion – Future initiatives on pain management wants and needsParticipant feedback was collected for each of the education forums. The feedback was positive with physicians requesting additional events to be held. Burnaby family physicians feel that this is a great forum to interact with Specialists and allow for feedback on hospital programs. It also provides an excellent forum for Burnaby Hospital specialists to promote the specialised services available to patients in the community.
Reducing Inpatient Echocardiograms
Project Champion: Dr. Sarah Ostler
An echocardiogram (Echo) provides information about a patient’s cardiac condition. This test is available to both inpatients and outpatients at Burnaby Hospital. Many inpatients remain admitted in the hospital waiting for their Echo test, unnecessarily extending their inpatient length of stay. About 43% of the echocardiograms performed at Burnaby Hospital are ordered for inpatients. In 2017, approximately 51% of these inpatients remained admitted an average of 5 days longer than their expected length of stay (ELOS); where some of them could have alternatively received their test as outpatients.
Having patients wait for tests as an inpatient slows down the flow of patients’ discharge, reduces the hospital’s bed capacity, puts pressure on staffing, and unnecessarily challenges the hospital’s resources and their optimal operational allocation.
To solve the issue, a team of four physicians set a goal to reduce number of patients receiving inpatient echocardiograms. They trialed a new requisition form to test its effectiveness. Feedback was sought from the physicians and booking clerks to identify opportunities to improve on both the “document” and the “booking" processes. The trial was then repeated with a larger group of physicians in specific departments, then spread throughout the entire hospital.
Changes Made
- Site-specific echocardiogram booking requisition form created
- Education to support improved patient identification for outpatient booking
- Adoption of an electronic booking process:
- Standardize the booking process
- Standardize the information provided to appropriately book an Echo
- Reduce potential for errors in the system by spreading it across Fraser Health
The Project Team: Teamwork was critically important in carrying out a project of this scope and successfully implementing change. Having a multi-disciplinary team provided the right amount and level of expertise that was needed to move forward in decision-making and tackle challenges. The hospital administration was supportive and heavily involved in the project as it involved operational process changes, and the following resources/departments were included:
- Medical imaging
- PCCs
- Clinical form services
- Clinical policy office
- BUH Admin
- PQI
- Unit ClerksProject Outcomes: The project was a major success as By June 15, 2019, the number of patients receiving inpatient echocardiograms at Burnaby Hospital decreased by 15%. A project poster presented at the Physician Quality Improvement conference won 1st place.
Enhanced Recovery After Surgery (ERAS)Project Champions: Dr. Gavin Gracias & Dr. Katherine Hsu

The delay until full recovery after major abdominal surgery/rectal-pelvic surgery and radical cystectomy has been greatly improved by the introduction of a series of evidence-based treatments covering the entire perioperative period and formulated into a standardized protocol. Compared with traditional management, Enhanced Recovery After Surgery (ERAS) represents a fundamental shift in peri-operative care. The ERAS-care pathways reduce surgical stress, maintain postoperative physiological function, and enhance mobilisation after surgery. This has resulted in reduced rates of morbidity, faster recovery and shorter length of stay in hospital (LOSH) in case series from dedicated centres and in randomized trials.
Changes Made (ongoing)
1. PDSA checklist on charts to collect data
2. Patient education post op – providing booklets/questionnaire
3. Implementation of ERAS protocols i.e carb drink and warming blanketThe Project Team: The ERAS project is a Fraser Health initiative. Facility Engagement funding enabled physician champions to develop a strategy to implement ERAS at Burnaby Hospital, to liaise with local nursing and administration to facilitate implementation of ERAS, and to oversee implementation. Monthly meetings have been held with physicians, hospital administration, and nurses.
Project Outcomes: The project is ongoing and has been successful in implementation of ERAS protocols. As this is a Fraser Health initiative, having physician involvement has been key in moving the project forward. The next steps include collecting data to determine its impact.
Crucial Conversations: Skills to Deal with Daily Challenges
Project Champion: Dr. Paul Johar

The Crucial Conversations course helps people master the skills needed to candidly and respectfully handle high-stakes conversations, achieve better results and enhance relationships. At Burnaby Hospital, 35 physicians and 5 administrative staff members attended this 2-day course. Both worked together to improve skills needed to engage others when addressing challenging issues. They learned to recognize when a conversation becomes crucial and received tools they could use to deal with daily challenges.
This course was originally offered in 2017 with 40 Physicians attending, and due to its popularity was brought back in 2019. As a result of the 2017 course, a crucial conversations club was started at Burnaby Hospital. This club enables physicians to identify challenges facing physician leaders and utilize the skills learned in the course to deal with them.
Project Outcomes: 40 learners participated in the course with 35 registering in the learning management system and 21 providing feedback regarding their experience. The course was well received by learners with 95% of respondents saying they were satisfaction rate with the course, that is was a worthwhile investment of their time and that they would recommend to a colleague.
Participants enjoyed the practical learnings in the course and enjoyed learning from knowledgeable and experienced faculty. They are ready to go back and apply the skills in the workplace by preparing for the difficult conversations and focussing on an outcome that is mutually acceptable to all parties. Learners expressed interest in future training regarding engaging others, managing people effectively and leading change.

Hospital-wide engagement creates a quality improvement culture
Read More Read LessQuality improvement champion Dr. John Hwang has teamed up with Royal Columbian Hospital administrators and frontline staff to build a culture of continuous improvement across the hospital.
The seed was planted in 2015 when Dr. Hwang and a team of frontline staff organized a “QI Day” for surgical services with the support of RCH administration. At the time, little was known about quality improvement activities around the hospital, so this was an opportunity both to teach participants about the importance of frontline engagement and to celebrate the accomplishments of unit-based QI teams.
Based on feedback from the inaugural QI day, the organizing team developed a series of frontline engagement workshops. The aim was simple: to teach those working on the frontline that continuous quality improvement is part of every provider’s job, and that making small changes within their scope of practice can collectively lead to big improvements in patient care. The following year, quality measures that had been stagnant for a decade showed notable changes in just about every area, ranging from surgical site and urinary tract infections to pneumonia.
Buoyed by those successes, the QI team (newly dubbed the "RCH QI League") expanded the effort right across the hospital in 2018 with a series of regular workshops leading into an annual QI Day in the spring. Physicians, front line staff and administration from all clinical services and departments contribute ideas, and learn how move them into action. With the support of Facility Engagement, physicians are able to take time to attend the sessions and provide ongoing leadership and mentoring. Participation has grown year after year.
Results are measured, and annual improvements are acknowledged, celebrated and spread across departments. “The first year we saw remarkable results. But the success was not a result of just one thing,” says Dr. Hwang. “It was because we focused on culture. So I see this ongoing effort not just as a QI Day, but a culture day – the recognition that everyone on the team has a responsibility to look within our personal scope and improve care as we can.”

Photo credit: Wendy D Photography/Fraser Health
Setting a Foundation for Engagement at RCH
Read More Read LessRecognizing Physician Leadership: Dr. Nora Tseng
Dr. Nora Tseng is an active family physician, and one of more than 400 physicians who care for patients at Royal Columbian Hospital (RCH). A major tertiary care facility, RCH is one of the oldest and busiest hospitals in BC. It shares patient services and a combined medical staff with nearby Eagle Ridge Hospital (ERH) in Port Moody.
Dr. Tseng recently retired from her position as President of the RCH-ERH Medical Staff Association, and after leading an impressive two-year effort to establish the Facility Engagement initiative at those sites.
In the beginning, how was the idea of Facility Engagement received at your sites?
It could not have come along at a better time.
Royal Columbian always had a very strong identity, a unique culture. Old-timers, including myself, remember what it was like. It’s tertiary referral centre, but had a community hospital feel. The medical staff was pretty tight-knit. Physicians felt a sense of belonging and ownership. They felt they had more influence. They were doing a lot of extra things, basically, on a voluntary basis. But got paid in kind, right? Because there was a regard, a respect. So doctors were interested.
Then the health authority embarked on program management to create some standards in the region where there were disparities. It had some positive outcomes, but in the process of everything becoming regionally-based, individual sites got sidelined.
It was difficult for physicians, including those who were at a medical staff executive level or in a leadership position. There may have been some nominal consultation, but without really any influence. Medical staff kind of checked out from a hospital engagement perspective. “You come in, provide good patient care and then you go home.”
But it’s going back now to more emphasis on the site. And now they want to know our thoughts, co-address, manage, solve issues. So the pendulum is swinging back.
Why did you step into the busy role of establishing Facility Engagement at the sites?
I kind of fell into it [after a predecessor secured incorporation approval]. I was warned by an experienced physician that it was going to take a lot of time. So I was not unprepared, but still, it’s always surprising how much time it takes.
But it’s a job that needed to be done. Doctors always want to do a good job. And so, you know, it’s like, “Well, you need to do A.” Okay, fine. You get A done, then “Oh okay, actually, there’s also B."
Also for a lot of physicians, it’s a matter of giving back to the hospital.
What did you tackle first?
That first year was very busy with setting up the working group and meetings and asking for representatives. At the beginning, there was a representative from maybe half of the departments in the hospital, and now we have one from just about every department. We all have different strengths, different backgrounds. Knowledgeable fellow executive and an effective working group are invaluable.
We also have two sites with a combined medical staff. Eagle Ridge as a separate site felt disengaged and disconnected. So that is one of the things that we’ve focused on, and it’s improving.
These last two years our main focus was to establish a solid foundation and organized infrastructure. The next two years, the new executive will likely work more in collaboration with site and health authority leadership.
How did physicians respond?
We knew we had to engage the physicians first to have a more coherent and cohesive community or identity, so we needed to get our own house in order. And we needed to set priorities in-house, that were relevant to our medical staff.
So we’ve held four engagement events, two per year. We had a reasonable response to our first meeting. People wanted to know what Facility Engagement was about. I still remember the questions: “What does engagement mean to you? What are the obstacles and opportunities?”
When we went around to see how people felt, there were some strong common themes from which we could pull to develop our vision and mission. And from those discussions we were able to set priorities: 1) communication and collaboration among physicians; 2) communication and collaboration between physicians and site/health authority leadership; 3) information technology; and 4) patient care and system change. We later added a fifth priority: physician wellness. We have a concern around physician burnout. Even before we had FE funds, a group of physicians were working on that.
We made our first call for proposals in May of 2016 and received 28; then 22 in the second round, and five in the third round. We discussed and scored them. Some didn’t actually align, so there was a learning curve for both the working group and the proponents in terms of what kind of projects we would fund or not. By the last round we approved all proposals. In total we have approved 33 and seven have concluded.
It is actually an engagement exercise in itself when a group of physicians come together to evaluate and make decisions about proposals.
What improved for physicians in those first two years?
I think for medical staff, there’s an improvement. There was a lot of unhappiness at the first meetings. One of the signs of success is that when we went into our third meeting, the tone was different. It was like, “we’ve already moved past that.” So depending on whom you talk to, how physicians see the health authority has improved somewhat.
You know, several of the projects are for physicians within or between large departments where there is a need for better communication and collaboration. So they can get together and really establish a relationship. And the feedback has been good.
As well, doctors are using the doctors lounge more often for coffee, and run into colleagues there in a more informal, relaxed environment. We don't always know who some of the specialists are as the older physicians retire and the new physicians come on. So even if you put a name to a face, it does make a difference when you need to consult about a patient.
As you move on and leave this work in others’ hands, what is shifting and what is making a difference?
Before, people would say, “we have a problem, we're pulling our hair out, we have some ideas, but nobody wants to listen.” And there wouldn’t be a way to approach the medical staff to co-address an issue.
Now, people come up to us and say, “We’re having some issue with this and that and can we use Facility Engagement funds?” We have the opportunity to say, “Yes, you can submit a proposal.” Medical staff have a venue, get compensated, and feel more validated for your time and effort.
And I think there are improvements just in terms of the relationships. Within the health care system, we’re looking beyond the transactional aspects which is more about finances, budget and "do you meet your targets and what's your length of stay" - to the relational aspects.
We know good doctor-patient relationships correlate with better patient outcomes. We feel good relationships between doctors and the health authority will lead to better patient care.

Left to Right: Dr. Richard Merchant and Dr. Kathleen Ross with Dr. Nora Tseng.
Below: Royal Columbian and Eagle Ridge Hospital physicians exchange Facility Engagement project updates, November 2017.

Renewing physician-health authority teamwork in Fraser Health
Read More Read LessThe spirit of teamwork that once defined the culture of hospitals is on the road to renewal through BC’s Facility Engagement Initiative (FE).
“When I look back to the ‘80s, I worked in hospitals where physicians were leaders and had good relationships with staff and administration,” says Dr. Dayan Muthayan, Executive Medical Director for Fraser Health. “Then through the '90s, we saw a deterioration of relationships universally when health care became more about the bottom line. Physicians started feeling pushed away or withdrew from decision-making and leadership,” he says.
“So it is encouraging now to see a resurgence towards engaging staff and physicians, while putting the patient in the centre and trying to make the health system better.”
BC is not alone. Across Canada, pressures on health care budgets, rounds of organizational redesign and continual cycles of change have taken a toll on collaborative relationships among physicians and health authorities. Here in our province, the Facility Engagement Initiative aims to change that. Medical staff in 67 hospital sites across the province – including all 12 Hospitals in Fraser Health – are involved in activities to improve relationships, communication and collaboration; as well as their working environment and ultimately, patient care.
This is welcome news. Meaningful physician partnerships are critical to support the delivery of quality patient care, as well as our work to create an integrated, patient-centered health care system. Physician collaboration and leadership will ensure that our efforts and results are effective. By leading change together, we can also enjoy a more rewarding work environment.

Forging partnerships in Fraser Health
In late fall 2017, 15 Fraser Health physicians – including specialists and family doctors –and 18 Fraser Health executive leaders from 11 different sites met to discuss ways to improve communication, renew supportive relationships, and create a culture of open dialogue.
The gathering was one of many combined operational and medical leadership gatherings taking place or planned across the province, where meeting face-to-face is an opportunity to connect personally, and share perspectives about barriers preventing engagement – as well as next steps. A few examples of perspectives shared by participants follow:
ON THE OPPORTUNITY: We need to recognize opportunities for positive change when they occur and seize them. They don't always happen all that often, or in ways that can change what is happening in a fundamental way. We don’t know if this one will, but this one could.
ON PHYSICIAN LEADERSHIP: Facility Engagement allows physicians the time and ability to spring forth with some of their creative, intellectual, and innovative problem-solving abilities.

ON RELATIONSHIPS: Engagement is just another way of saying ‘relationships.’ The most important part of making effective change that benefits both and physicians and health authority and ultimately patients, is about having relationships you can trust.
ON BUILDING TRUST: It is an evolution. In the beginning, we needed to be reassured this was real, so activities were mainly doctor-focused. Then we moved to start projects to improve processes and make collaboration better. That has evolved over many months to inviting the executive director [of the hospital] to our meetings.

ON DECISION-MAKING: Consultation may not always mean being involved in co-designing decisions. Decisions are made in many different ways. We make assumptions and may think that our opinion did not matter. It is important to understand the method used.
We hit our stride when we moved from a checkbox approach early on, to now inviting the administration / executive to the working group for meaningful discussions.ON BARRIERS TO ENGAGEMENT: Administrators come and go, and doctors stay. The constant shift is a huge challenge. Meaningful succession planning is needed both with the health authority and physicians when people leave, to retain the knowledge and institutional memory and get new people up to speed faster.

ON COMMUNICATING INFORMATION: It is important to communicate in a more timely way, and use multiple channels to distribute information. But whether by text or personal e-mails, it is just the transaction. It supports, but doesn't speak to the partnership we are trying to build. The relationship is the transformational part of this.
ON SUPPORTING GOOD ENGAGEMENT: Health authorities as well as physician groups need to model a culture of open discussion and transparency and develop solutions to engage physicians when that is not always possible [such as with union confidentiality matters]. We need to involve site administration early in meetings and hold joint partnership meetings with MSAs, health authorities and where needed, Divisions of Family Practice, to talk about collaborative goals.
Fraser Health Facility Engagement Activities

As of January 1, 2018, physician groups have formed in all 12 acute care sites where physicians and other medical staff members are now actively engaged in more than 100 Facility Engagement projects, including many collaborative activities that involve site administrators and staff.
It is early days, and laying a strong foundation of relationships and communication is an important first step to determine how Facility Engagement evolves.
“We're proud of how far we have come in just a year’s time, from setting up legal structures to making significant impacts in the lives of physicians, health authority representatives and patients,” says Dr. Muthayan. “It will be exciting to see where we could be over the next two years.”
- Interior Health

Promoting Gender Equity in Medicine and Leadership
Read More Read Less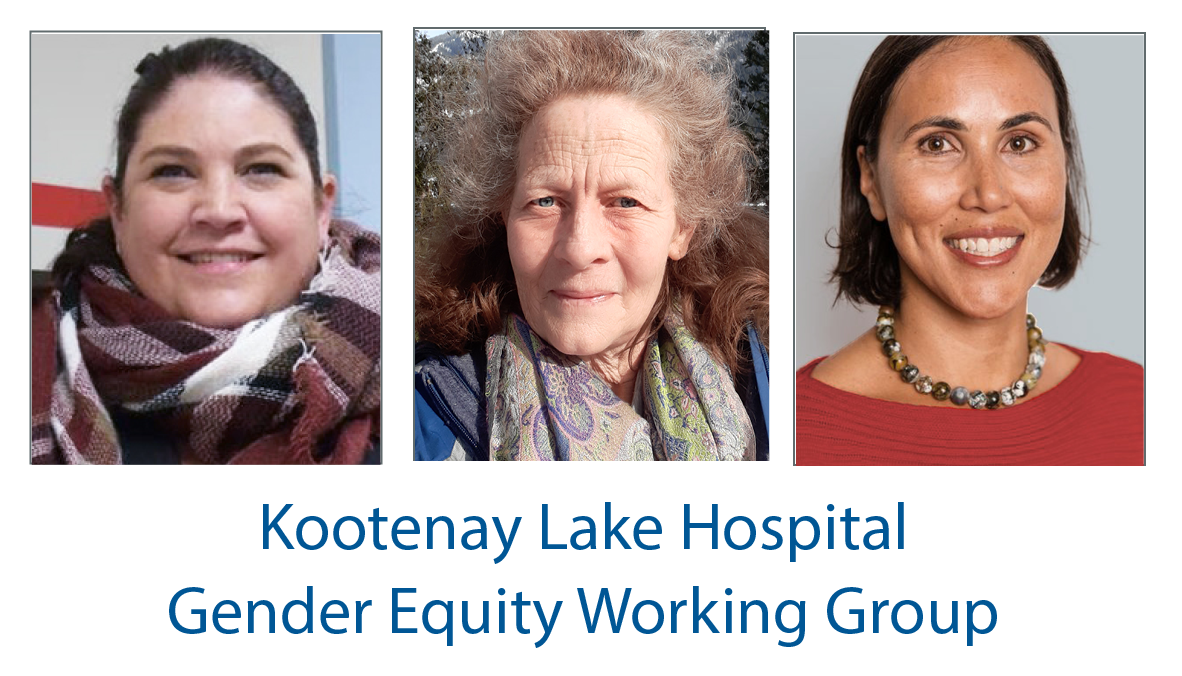
At Kootenay Lake Hospital (KLH) in Nelson, the MSA's Gender Equity Working Group is introducing strategies to shift to a more supportive, equitable environment for women in medicine, that is also more conducive to leadership. The group is also working with neighbouring hospitals to elevate and promote strategies at the regional level.
As the number of female physicians grows, more women have the opportunity to take on leadership positions and have a greater influence in health care decisions. However, female physicians in medicine experience gender equity challenges in both leadership and clinical opportunities.
Read about the KLH strategy here>

Building a culture of respect, safety and support in Interior Health
Read More Read LessAcross Interior Health, physician leaders from MSAs, divisions and the health authority are creating a ‘community of communities’ built on a culture of respect, safety, and mutual support. A region-wide leadership forum is serving as a conduit for issues, wellness, anxiety and hope – while forging thriving relationships that are bringing people together around shared priorities. They are using strategies that can also be effective at local level hospitals.
The genesis for change started in 2017, when the Doctors of BC Health Authority Engagement Survey results showed that just 28% of physicians were satisfied with Interior Health as a place to work – and revealed a ‘lack of effective communication’ as one root cause. Health authority physician leaders Dr Mike Ertel, Vice President Medicine & Quality, and Dr Harsh Hundal, Executive Medical Director for Physician Engagement and Resource Planning – decided to do something to fix this.It would be no small feat to build trust and relationships across hundreds of diverse rural and urban communities, 22 acute care sites, 34 emergency rooms, 150 care facilities, and a multitude of health care services. Having simple meetings would not be enough: they needed to change the underlying culture.
Changing the culture starts with listening
Their key focus was to establish a psychologically safe, supportive, and inclusive environment for physician leaders to connect and communicate openly with each other and the health authority. To enable this, Drs Ertel and Hundal made a commitment about their own role as senior health authority leaders: to be present, consistent, responsive and transparent; and to serve physicians with gratitude – and lead by example.
They began to listen – applying these principles to many discussions that followed – and by 2020, had made inroads to improve trust and relationships. When COVID-19 hit, they were able to draw on groundwork they had laid for a faster, coordinated regional response to the crisis. At the same time, they accelerated a key communication strategy that has since brought everyone even closer together.
Zooming to the next level: a safe, supportive environment
What started as weekly Zoom meetings to elevate the level of coordination and support for physicians during the pandemic, has shaped up to be so much more. A robust, effective virtual forum has emerged where MSA presidents, division leaders and their directors, chiefs of staff, health authority executive regional and quality leaders, operational leaders and guests connect regularly in a safe space.
Each group contributes to a shared agenda with respective burning issues, making it worth everyone’s time to attend. “We have talked about COVID. We also talk about wellness. We have talked about gratitude, and our relationships with administrators and our staff. We’ve talked about racism,” said Dr Ertel. “Attendance has increased because we’re not nibbling around the edges. These are some pretty big topics we’re discussing, and often controversial.”
At the same time, they are integrating the building blocks of respectful and thoughtful exchange to create an inclusive space where people feel safe to speak up.
“It’s about creating a psychologically safe environment for individuals to be vulnerable, to say they don’t know, or bring up concerns and know they are not going to be judged.” - Dr. Harsh Hundal
Dr Hundal notes that people wouldn’t normally speak were now willing to speak up, so it is not just the dominant personalities. And putting a human face to issues being discussed is allowing problems to be solved before they become a crisis and building the relationships needed to work effectively.
It is also levelling the playing field by removing silos and enabling mindful cross-pollination for problem-solving. Dr Ertel says, “Chiefs of staff and MSAs from the larger sites to hear the concerns from our more rural sites. And it’s really beneficial that our rural sites feel heard.” An added advantage is seeing physicians and MSAs connect after meetings to share advice.
Sharing up, down and across
Dr Ertel emphasizes that it is invaluable for the organization to hear what’s happening on the ground in smaller communities. “What are people talking about in the supermarket in Williams Lake or in Creston or in Fernie?”
It is equally invaluable for physicians to hear about what’s going on provincially. Drs Ertel and Hundal share news back and forth with and from other operational, provincial and partner meetings. That helps medical staff to learn and understand how the health authority and health care system works and how they can contribute to it – which is essential for robust and sustainable engagement and responses.
“Doctors get a bit of a tenth-floor view instead of the second-floor view, and they really appreciate that,” - Dr Mike Ertel
In addition to agenda items, round table discussions uncover ideas and concerns, determine what to escalate, and identify what supports can be offered. Dr Ertel says, “If we don’t know we’ll say we don’t know. If there is something that we can’t move along, we’ll admit it. We’re honest about our struggles.”
This attitude helps to build credibility and trust, while shifting and broadening the conversation. “We can be more future oriented,” says Dr Hundal. “What is the positive future we want to build, as opposed to what we don’t have? It’s less about anxiety and helplessness and more about hope and what we can do.”
Meetings are well-attended by the physician leaders, and generally held in the morning before clinic hours on a weekly, monthly or as-needed basis. Larger, grand-round style virtual meetings that include even more physicians at large – have maxxed out Zoom capacity with as many as 499 attendees.
Increasing physician satisfaction
It’s all fueling a culture change. Results of the most recent Health Authority Engagement Survey reveal a huge increase in physician satisfaction in Interior Health, moving from 28% to 65% in three years. “That is a lot of work, a lot of face time, and a lot of listening,” said Dr Hundal.
It speaks volumes to work that that will continue, ultimately to provide quality patient care within a highly satisfied working environment. Already, it has allowed for a more efficient response to Covid-19, and is generating similar responses for anti–racism work. “It really does pay off for the organisation and I think it saved lives at the end of the day,” said Dr Ertel.
Dr Hundal sums it up, “It comes down to creating community at the local level and healthy authority-wide. Message number one, you’re not alone. Message number two, the anxieties that you feel, there are others who feel it as well. And message number three, we can get through this together. We can work out solutions. We can support each other. We may not solve everything, but we’re here together.”
Facility Engagement is an initiative of the Specialist Services Committee, one of four joint collaborative committees that represent a partnership of the Government of BC and Doctors of BC.
Kootenay Lake Hospital: From the ER - Love is Also Contagious
Read More Read LessThese are challenging times in BC, and staying positive is more important than ever.
That’s why emergency physician Dr Linda Johannson took action to try to uplift her own spirits, and of her colleagues.
“Everyone was feeling stressed and real fears about what was to come,” says Dr Johannson. “I didn’t realize how deeply it [the Covid-19 pandemic] all was affecting me until one night on shift when I snapped at a nurse, something that is very out of character for me. She snapped back, also out of character for her, and we had a terrible shift together.”
After apologizing to the nurse and reflecting, Dr Johannson realized that everyone was feeling anxious, and this was affecting how they treat each other.
She acknowledged she wasn’t doing okay, and attended an online meditation session. The facilitator mentioned that a colleagues’ display of an anxious, fearful attitude is contagious and can spread to the whole team, and the reverse is also true.
This sparked the idea for the “Love is Also Contagious” campaign.
“I wanted a way to remind people that, because of the fear we are all experiencing, our behaviour may not be consistent with the way we know each other to be,” says dr Johannson. “We can recognize that in each other and in ourselves, offer forgiveness, and choose to behave in a loving way rather than react to the stress that is going on.”
Dr Johannson shared the campaign idea to spread love, not fear, as an attitude at work with her colleagues. With their overwhelming encouragement and funding from Facility Engagement, an initiative of the Specialist Services Committee, Dr Johannson started to work on the campaign.
She asked a friend who is a graphic designer to morph an image of the coronavirus into a heart. They turned this friendly image into buttons and stickers and a downloadable window sign.
In full support of the campaign, the Kootenay Lake Hospital (KLH) administration sent a facility-wide email introducing the campaign and encouraging staff to wear the image as a visual reminder to act from a place of love.
Keeping the momentum going, Dr Johannson regularly distributes “Love is Also Contagious” pins and stickers around the hospital during different shifts.
“I can really feel the positive energy when I show up with my bag to hand out some love,” says Dr Johannson. “It’s been a lot of fun, and a side benefit has been that I feel much more positive about weathering this storm, both individually and as part of a top-notch team in KLH Emergency.”
Help spread the love. Download the “Love is Also Contagious” window sign.


Courage and community come together to improve surgical quality and safety
Read More Read LessDr Michel Hjelkrem, an orthopedic surgeon at Kootenay Boundary Regional Hospital took what some might consider drastic steps to reduce surgical site infections – he stopped doing joint replacements. Then his four partners joined him. This was in late 2017 and for the next two and half months, they embarked on a mission to improve surgical standards. And while it wasn’t always an easy road, it turned out to be one of the best decisions they made to lower infection rates well below the national average.
The hospital administration was initially reluctant to delay patient procedures. But with support from SSC’s Facility Engagement Initiative – the physicians were able to initiate meetings and discussions to get everyone working towards the same goal, which included taking a pause and making some changes. At the time, infection rates were about 2.8%, compared to the national average of 1% to 2%.
“Morbidity and mortality associated with infection is a big concern,” said Dr Hjelrem. “If you get an infected joint replacement you’re looking at a minimum of three more surgeries, extended time in the hospital, extended intravenous use, complications, toxicity. It’s difficult to get rid of.”A hospital-wide effort

The entire hospital - from specialists and managers, to nurses and students, to cleaners and engineers – was engaged to join the effort. “It takes a community to prevent infection,” he said. “We needed everybody to be involved.”
The first step was to have the hospital upgrade its ventilation system. In the four ORs, air ducts were cleaned, a HEPA filtration system installed and room temperature, humidity and pressure became better controlled.
A new leader was secured for Medical Device Reprocessing (MDR), responsible for instrument cleaning. Surgical staff reviewed their processes and tightened up their actions. An expert reviewed orthopedic procedures over several months and provided education and awareness.
Dr Hjelkrem and his team also worked with GPs to ensure patients achieve the best health possible prior to surgery by developing criteria that included optimizing weight and reducing risk factors related to smoking and dental health. They also looked at how post-op patients were cared for - ensuring they recovered in a different room from other infectious patients - and introduced software to prevent deep vein thrombosis.
Going the extra mile
In January 2018, the changes were in place and the surgical program restarted. For a year after that Dr. Hjelkrem continued to advocate for one more addition which is known to substantially decrease infection rates. The process involves ‘decolonization’ or sterilizing the nose with a laser and special ointment, as well as using special wipes customized for pre-op patients. At about $50 per patient, it took some convincing to have the cost of the procedure covered. But given the average cost of an infected joint replacement in Canada is about $30,000 to $50,000. “By preventing one infection, we pay for our program for two years,” Dr Hjelkrem noted.
Trail became the second hospital in Canada to introduce the procedure, and Dr Hjelkrem notes that other hospitals noticed and expressed interested in adopting it as well.
Big results
The results speak for themselves – infection rates dropped well below the national average, to 0.4% after just one year – and less than six months after the procedure to sterilize pre-op patients was implemented – the infection rate dropped again to 0.2%. In addition, a lot of actions taken weren’t confined strictly to orthopedics – so the overall infection rate for the hospital has also dropped by 50%.
As results revealed themselves, others jumped in to join the effort. “We started getting suggestions from even more people coming up to me and and saying, ‘Hey, what else can we do?’” Cleaners suggested that iPhones be kept out of the OR. Engineers offered to change filters during the smoky summer months. Nurses wanted CPAP equipment reviewed. Even patients got involved, with suggestions like “I’ve had this band on my arm for a week, shouldn’t it be cleaned?”
“There is no doubt that most important component to our success was the engagement of everyone in the hospital – no one was left out,” said Dr. Hjelkrem. “It’s been a really, really positive experience. There have been some heartaches and bumps along the way, but the end result is that we’re achieving a large part of what we set out to do.”
Happy, safe patients
Best of all: improved quality and safety. “We have had such great response from the patients. It’s been unbelievable. There’s been a lot of really good stories that have come up because we’ve been so diligent about optimizing our patients. We’ve become a hospital that people now want to come to to have their surgery,” he said.
“A local retired physician recently told me that he’d want his wife to have her knee replaced at KBRH because we have such a reputable infection prevention program.”
MSAs: Your Engagement Partner can connect you with this project team if you wish to get more information.

Recognizing Facility Engagement excellence in Achievement, Partnership, Innovation, and Teamwork
Read More Read LessCelebrated at FEI Interior Regional Showcase and Networking Event
Last year, Interior Health Facility Engagement Initiative (FEI) facilities participated in the Site Review and Reporting Process to share feedback about the work being done and to develop plans for the year ahead. The calibre of work and projects was outstanding, with many of the facilities’ projects and initiatives truly exemplifying excellence.
MSAs, health authority partners, and project staff were brought together to recognize efforts that have inspired, sparked change, and brought the Facility Engagement Initiative to life in the Interior Region. Four of these facilities were further recognized by Facility Engagement for Excellence in Achievement, Partnership, Innovation, and Teamwork.CERTIFICATE OF EXCELLENCE IN ACHIEVEMENT – recognizing a project/initiative with robust evaluation showing measurable and significant results, aligning with the goals of the FEI’s Memorandum of Understanding.

The Kootenay Boundary Physician Association (KBPA) and Regional Hospital (KBRH) was recognized for their support of progressive work that, through the power of engagement and perseverance, improved patient outcomes in their facility.
The post-operative infection rate at KBRH was 2.8% - well above the national average. Orthopedic surgeon Dr. Mike Hjelkrem, along with four of his surgical colleagues, set out to improve it. Through engagement with stakeholders at all levels and departments, from cleaners to engineers to health service administrators, the team identified a multitude of improvements that reduced infection rates down to 0.2%.
CERTIFICATE OF EXCELLENCE IN PARTNERSHIP – recognizing strong successful partnership between medical staff and Interior Health – involving early and often collaboration.
Shuswap Lake General Hospital (SLGH) was recognized for their leadership in collaboration and partnership.
 This group has gone above and beyond to collaborate with local, regional and corporate Interior Health stakeholders. The SLGH FE working group has developed an ‘open door policy’ for their meetings which encourages a diverse group of Interior Health members to attend. They have developed a strong partnership with local and regional Interior Health staff by including the most appropriate IH representatives for solutions, challenges and ideas. The IH Senior Medical Director and Health Service Administrator have partnered with the SLGH physicians to collectively work on facility challenges, using the 2018 FEI Interior Regional Meeting 10 Recommendations as a foundation for change.
This group has gone above and beyond to collaborate with local, regional and corporate Interior Health stakeholders. The SLGH FE working group has developed an ‘open door policy’ for their meetings which encourages a diverse group of Interior Health members to attend. They have developed a strong partnership with local and regional Interior Health staff by including the most appropriate IH representatives for solutions, challenges and ideas. The IH Senior Medical Director and Health Service Administrator have partnered with the SLGH physicians to collectively work on facility challenges, using the 2018 FEI Interior Regional Meeting 10 Recommendations as a foundation for change. INNOVATION AWARD - recognizing a new/creative approach to a complex problem accomplishing positive change.
 The partners at the Creston Valley Hospital were recognized for their work to create a new maternity clinic in the region.
The partners at the Creston Valley Hospital were recognized for their work to create a new maternity clinic in the region.Eighteen months ago at Creston Valley Hospital, three physicians providing maternity services – Dr. Barry Oberleitner, Dr. Crystal Campbell, and Dr. Karen Persad - approached Interior Health with a proposal to develop a clinic within the hospital and health centre that would integrate maternity services and include public health nurses. As a result, the multi-disciplinary Maple Maternity Clinic opened at Creston Valley Hospital this year. Physicians, Interior Health administrators including Acute Health Service Administrator Erica Phillips, Site Director Deb Austin and Site Manager Carolyn Hawton, public health nurses, staff and community partners, worked together to transition maternity care from two clinics in Creston to a centralized clinic at the hospital.
TEAMWORK AWARD - recognizing a project/initiative that has featured large involvement of the working group, physician leads, and larger MSA involvement, demonstrating excellence in teamwork by physician engagement.
Royal Inland Hospital (RIH) in Kamloops was recognized for outstanding efforts in teamwork, engaging significant and diverse members of their medical staff team.
 With a physician membership of over 300, the Royal Inland Hospital Physician Association has worked tirelessly to engage their medical staff so that they can prioritize patient care needs. 60% of MSA members - representing every department at RIH – are either leading or participating in over 44 FEI activities. Physicians stepping into leadership roles are supported and united with other medical staff and have the ability to bring things to the forefront with administrative leaders. In 2018, RIHPA participated in the formation of the Thompson Medical Alliance to align physician initiatives in the Thompson area that includes: Facility Engagement, Divisions of Family Practice, Practice Support Program, Physician Quality Improvement, IH Quality Improvement, and IH Research.
With a physician membership of over 300, the Royal Inland Hospital Physician Association has worked tirelessly to engage their medical staff so that they can prioritize patient care needs. 60% of MSA members - representing every department at RIH – are either leading or participating in over 44 FEI activities. Physicians stepping into leadership roles are supported and united with other medical staff and have the ability to bring things to the forefront with administrative leaders. In 2018, RIHPA participated in the formation of the Thompson Medical Alliance to align physician initiatives in the Thompson area that includes: Facility Engagement, Divisions of Family Practice, Practice Support Program, Physician Quality Improvement, IH Quality Improvement, and IH Research.Congratulations all!

The changing landscape of engagement in Interior Health
Read More Read LessFacility Engagement Regional Showcase and Networking Event, Kelowna - October 22, 23 2019
What a difference two years has made.
Last month, Interior Health Medical Staff Association (MSA) physicians, project leads and health authority partners joined together in Kelowna to share Facility Engagement experiences, knowledge and strategies, and to celebrate the progress that has been made since they first gathered two years ago.
At that time, the tone was decidedly different. Physicians expressed frustration about their relationship with their health authority, and according to the 2017 Doctors of BC Health Authority Engagement survey, only 28% of them felt that Interior Health (IH) was a good place to practice medicine. IH leadership listened, and responded with a genuine commitment to make things better.
Two years later, the initial sentiment is turning around. Now, 51% of physician respondents to the 2019 Doctors of BC Health Authority Engagement survey say that IH is a good place to practice medicine.
So how did things change? A combination of factors. In addition to committed regional leadership that supports a culture change, local Medical Staff Associations have been working enormously hard to improve communication, trust and collaboration amongst physicians and health authority counterparts in their own hospitals and health regions.
Dr. Harsh Hundal, Executive Medical Director for Interior Health Physician Engagement & Resource Planning, says a key ingredient is driving change.
“What this speaks to is relationships – seeing each other as people. Relationships underlie everything. We’re on a journey together. You don't engage facilities, you engage people, and in order to engage people you need to see the world through the complexity of what they deal with.
Everybody wants to do a great job. But we recognize that we have been working silos. Let’s reach out to partners, get to know them, ask them how they are doing.”
On that growing foundation of relationships, MSAs from across Interior Health have been able to collaborate with their health authority counterparts in ways that were not possible in the past, and to successfully advance dozens of improvements at their sites.
For the 27 physicians, 21 project staff, and 18 IH administrators who attended the October 23rd event, the opportunity to share experiences and learnings was buoyed by optimism and energy. While there is still a lot of work to do, all signs are pointing towards a healthy, growing culture of engagement across Interior Health.

REFLECTIONS FROM EVENT PARTICIPANTS
“Changing culture is a slow process. You have to make efforts to change it. And it is totally worth it.”
“I didn't think I would be interested in these leadership roles, but as I got involved I am quite interested, and it really gives me an idea of how things work. It is not useful to just sit in your office to complain about things - it is worthwhile to come out here and change things.”

“When in leadership, don’t be afraid to show enthusiasm and ask questions. Step forward and ask questions: how does this work?”
“Face to face and networking – being present in the room together – whether having conversations together at coffee, dinner, or social activities are equally as important as standing in front of a room with a mic.”

“We are hearing over and over again you have to have that relationship piece built before you can make any real change or expect any work to stick. Solidifying those relationships is the foundational work that needs happen before any real change can be expected.”
"Engaged physicians who are excited about where they work and making it a better place are the best recruits for this work."

"The most exciting part of this shared learning experience was the honest, open, two way dialogue around major issues facing the physicians delivering care locally with the Health Authority leaders. The need for transparency and conjoint identification of problem areas, barriers and limitations were major themes. The most inspiring outcome was a clear agreement to continue collaborative discussions and shared decision making moving forward." (Dr. Kathleen Ross, President, Doctors of BC)


Widespread engagement jumpstarts overcapacity solutions
Read More Read LessAdvancing a Vision for Change
Most hospitals in BC experience over-capacity and access and flow challenges to varying degrees, and have held multiple meetings over the years to look at solutions. But despite best intentions, many of those ideas stall after everyone gets back to their busy jobs.
Dr Charles Casselman, Chief of Staff for East Kootenay Regional Hospital, set out the change that.
As big vision thinker who works behind the scenes, Dr Casselman knew that the first step to success was to get the right people at the table. Physicians are rarely able to attend meetings during clinical hours, yet their voice is critical to the conversation to ensure that plans involving patients are workable.
So he leveraged the Facility Engagement opportunity to bring together the brightest minds for a pivotal planning workshop in May 2019. While Dr Casselman rallied the physicians, Erica Phillips, the Interior Health Acute Health Service Administrator for the East Kootenays, worked to have health authority administrators to attend events after hours.

Bringing stakeholders together: an abundance of ideas
The May forum – attended by 78 people including 27 physicians, 25 Interior Health representatives and other stakeholders – not only generated an abundance of rich ideas and perspectives, it set out foundation for an ongoing collaborative effort. A third party consultant firm, Reichert and Associates, took the feedback and along with data research and patient and stakeholder interviews to set out some longer term recommendations.
On June 24, the same group came together again to hear recommendations from Reichert. Participants were energized to meet again and consider the opportunities ahead. Even local elected officials attended, excited to see what might change for people living in the community. Now the group will plan out next steps to action the recommendations.
Support for change: not just off the side of the desk
A key missing link – not available in the past – was within reach: a dedicated support team with MSA project manager Jill Bain and administrative help was waiting to jump into action to break the changes down into manageable steps, and to keep them moving along among the partners. And while there is still much work ahead, there is plenty momentum around the shared vision that is propelling the plan forward. Stay tuned.
“Trying to solve the problem of too many patients in your hospital absolutely has to involve everyone finding solutions. This is a great jumping off point to use some resources we have we didn't have before to get us someplace we couldn't have gone otherwise.” - Dr Charles Casselman
MSAs who wish toget a copy of the Reichert overcapacity recommendations can contact: ekrh.mss@gmail.com
WATCH VIDEOS: Collaboration and change at EKRH


United voices improve physician engagement across Interior Health
Read More Read LessThere has been a major shift in physician engagement across Interior Health in the last year.
With physician-administrator dyad partnerships, quality improvement projects, and facility engagement initiatives, physicians have strengthened relationships with administration, are more connected to resources and training to improve the work environment, and have established activities and strategies to improve areas of need at the site level.
“I am incredibly humbled by the work of our medical staff across IH. They are taking the time to have meaningful and constructive conversations about the things that matter and then making positive changes. It is their passion and drive that is having the greatest impact to the work culture, the patient experience, and the quality of care.”
- Dr. Harsh Hundal, Executive Medical Director, Physician Engagement and Resource Planning
Read full article (originally published in the Interior Health magazine, page 6) >

Physicians ‘unstick’ a project to introduce local treatment options
Read More Read LessThe Facility Engagement Initiative has identified and implemented many health improvement projects in a number of hospitals across BC, but sometimes its value is in helping ‘unstick’ a project – like one that languished for about two years. The project - to develop a uterine fibroid embolization (UFE) program within the Royal Inland Hospital (RIH) in Kamloops.
A similar program has run for about 20 years in the Lower Mainland. Women in Kamloops with severe symptoms caused by fibroid tumors whose other treatment options were unsuccessful or more invasive faced the decision of having a hysterectomy or travelling to Vancouver for a specialized minimally-invasive procedure of fibroid embolization.
Fibroid embolization treatment
The fibroid embolization treatment involves puncturing an artery in the body and having an Interventional Radiologist guide a catheter into the uterine arteries and injecting tiny particles that float into the uterus to block off the blood supply to the fibroid tumor(s) – eventually shrinking or killing them. The procedure is done in an angiographic suite in the Radiology Department and only requires an overnight stay once completed.
Championed in the region by Dr Michael Burns an Interventional Radiologist – a proposal was put together three years ago in conjunction with Dr Brooke Cairns of Kelowna General Hospital who was also interested in establishing a UFE program.
The proposal was first submitted to the Interior Health’s (IH) Health Technology Assessment Committee, who approved it in 2016. It was then that Dr. Paula Lott, a Gynecologist and committee member with the RIH Physician Association suggested to Dr Burns that Facility Engagement (FE) could take this on as a project. However, by 2018 final approval and funding from IH was still not moving along.
Collaboration gets things moving
It was with Dr Lott’s help that the project got moving again connecting Dr Burns with the right Interior Health administrative people. At the same time, the Ministry of Health were looking for ways to free up OR time. Establishing the UFE program was one way to help because it reduced the need for hysterectomies to treat this issue.
Soon Dr Burns found himself connecting and partnering with IH Peri-Operative Management Committee, local administrators, managers and gynecologists. “In particular IH administrator Sue Gardner-Clark was very helpful once we got the greenlight – she helped get the local process off the ground.”
Since it is a new procedure, FE also funded the time Dr Burns needed to engage in these meeting, write protocols, determine steps to educate IH staff in the radiology department, technicians, nurses, and daycare surgery staff; as well as write new post-procedure orders and protocols, patient advice sheets and so on. Dr Burns said, “Staff were very interested and open to it, but they wanted to be sure the procedure was safe and that they were appropriately trained to deal with any complications.”
Taking an extra step for safety and quality
As a new program, Dr Burns also followed a new technique by puncturing the left radial (wrist) artery rather than the femoral artery at the groin. This is safer for the patients and doesn’t require them to stay lying flat during post-operative recovery. The program began in April 2019. It is estimated that between 20 to 30 patients a year could eventually benefit from this new and less invasive technique.

Proactively supporting physician wellness at Royal Inland Hospital
Read More Read LessPhysician wellness and burnout are often common issues discussed among the physicians involved in Facility Engagement. At the Royal Inland Hospital (RIH) in Kamloops, an annual RIH physician engagement survey first addressed the need for a physician wellness initiative. Contact with Doctors of BC’s Physician Health Program eventually led to the recommendation that RIH establish a Physician Wellness Committee.
Established in late 2018, the committee is supported by the Royal Inland Hospital Physician Association and led by Dr Megin Fong. Dr Fong believes in fostering physician wellness because “you can’t really help your patients, if you are not taking care of yourself first.”
The committee’s activities included conducting a needs assessment survey, which found physicians wanted particular attention paid to team-building, support and recognition.
As a result, the committee developed three distinct programs: R.I. Health, Recognition @RIH and Asclepius Peer Group. While R.I. Health encourages team-building through a variety of educational/informational workshops - for example billings and audits - and Recognition @RIH highlights the achievements of physicians in the hospital and community – the Asclepius Peer Group pilot program is all about team-building and support.
Asclepius Peer Group - A safe, anonymous environment
The peer group pilot program held weekly 1-1/2 hour meetings over an eight-week period with a maximum of 10 physicians. During the meetings, physicians discussed their challenges, critical incidents, impact of their work and so on. The meetings were facilitated by a professional and anonymity was maintained so physicians had a level of safety and trust that what they said remained ‘in the room’ and confidential.
The first cohort of physicians have recently finished the program and feedback included a positive response to the impact of these meetings, which promoted deeper connections among the participants.
“Based on the experience I had attending the Asclepius Peer Group; incorporating balance into my own practice of wellness would include fewer late nights in office and more relaxing activities.”
A second eight-week cohort begins in October and based on feedback from the first physician group – the focus will be to provide physician participants with tangible skills and exercises to maintain wellness in both their professional and personal environment.
Eventually, these groups will help address and support physician wellness by identifying strategies and actions that will shift the culture and alleviate physician burnout well into the future.

Kelowna General Hospital ER orientation & mentorship initiative
Read More Read LessLast year, the Kelowna General Hospital Emergency Department (ED) was busy hiring new locums and permanent Emergency Medicine Physicians.
Dr. Brandy Bursey, an emergency room physician, recognized that there was no formal orientation or mentorship program in place to prepare the new recruits for working in the hospital’s busy ED. Wanting new recruits to be prepared and welcomed into this new environment, Dr. Bursey, together with her colleagues Drs. Karla Tujik and Jennifer Williams, received funding from the Facility Engagement Initiative and began work on developing an orientation manual for new staff.
The manual covers a wide array of “need-to-know” information which has been well received by new Department members.
In addition, the project team assigned a mentor to each new ED physician to welcome them, and have a go-to person to connect with should they have questions. This idea helped to improve the work environment for new Emergency Medicine Physicians, supporting them to be successful in their roles.
Other medical departments have been invited to create an orientation manual if they wish.
(Originally published in the KGH Physician Society Newsletter)

Facility Engagement helps Creston centralize maternity care with a new maternity clinic
Read More Read LessThree physicians have led the way to a collaborative effort between physicians, interior health administrators, nurses and staff to centralize maternitycare in the Creston area.
As a result, a new clinic was established within the hospital to integrate maternity services and bring multidisciplinary teams together to provide pre, peri and post-delivery maternity care.
Funding for the collaborative effort was provided by Facility Engagement, a partnership of the government and Doctors of BC.
Read the full news release here.

Coffee, Colleagues and Gratitude Cards
Read More Read Less~~When staff arrived at the Kootenay Lake Hospital on the morning of Monday July 30, they smelled coffee and saw their colleagues gathered around a café that didn’t exist before. The environment had changed to a warmer and more welcoming one. Everyone was encouraged to join, and were served a cup of coffee and a muffin before writing on ‘gratitude cards’ about what and who they appreciated in the hospital.
Acknowledging the fact that the staff at the Kootenay Lake Hospital had not come together as a group of colleagues over the last two decades, Dr. Gregory Hand, the Facility Engagement Working Group Chair, thought it was time. A few months prior when elected, he started meeting with individual physicians during lunch. After hearing input from those meetings he realized that real engagement wouldn’t be possible without creating a positive work environment and opportunities to bring together staff and physicians in casual environments.Dr. Hand can be seen in the above picture using an espresso machine to make coffee. After reviewing their strategic engagement plan, the MSA realized that they did not have a place to meet, like a lounge or a café, and came up with a brilliant idea of having a casual pop-up café. They named it “Appreciation Café” and invited everyone at the hospital - from nurses to physicians, clerks, patients and cleaners - to join.
As Dr. Hand recalled, “When we thought about who we were trying to engage, we initially thought of medical staff peers. But then we also realized that if we want to bring changes to the hospital environment, we had better consider engaging other people like the administrators, the staff, as well as the public.”
Two-hundred appreciation cards were collected, attached to banners and displayed at the main entrance of the hospital. Here are some of the messages:
- “Management cares about staffing needs, and patient concerns, dilemmas and stressors.”
- “Supportive, hard working environment that also has time for a smile and a laugh.”
- “I am grateful for being part of such a healthy, happy, joyful team. Great personalities here at KLH.”As a result of this initiative, “people were really happy,” Dr. Hand said. “All the staff seemed to feel connected. There was a sense of camaraderie. It was pretty inclusive and a good starting block to build on.”
The MSA held two more pop-up cafes with the support of Facility Engagement. The Interior Health administrator, Thalia Vesterback is now looking for a permanent space and contractor for a coffee shop at the hospital.
Facility Engagement is one of nine SSC initiatives that helps build relationships and assists in finding effective solutions for medical facilities across BC.

Big challenges sometimes find easy fixes
Read More Read Less[Picture-from left to right: Dr Allison Howatt, General Practitioner at SLGH, Peter Du Toit, SLGH Hospital Administrator]
Working in a small, rural hospital like Shuswap Lake General Hospital (SLGH) can present some unusual challenges. Sometimes these challenges have an easy fix – particularly when the right people get in the room to talk about them. Facility Engagement (FE) is all about getting the right people together to collaborate and improve both their relationships and patient care.
Dr Allison Howatt, a GP at the SLGH with enhanced OB/GYN skills saw an opportunity to fix a growing issue around care for babies born with premature lungs requiring respiratory support. The hospital only had one way to deliver this care - through a neo-puff system, which required a health care provider to physically hold the equipment in place to maintain pressure – often for many hours until the infant is transferred to a higher level of care facility. The process could be both physically draining and time consuming for healthcare providers with so many other responsibilities.
When an infant transport team member asked Dr. Howatt, “Why don’t you guys have a proper C-PAP machine?” she took up the challenge, and put it on the table as part of capital planning considerations for Interior Health. A C-PAP system provides automatic seal and support needed for pre-mature newborns’ respiratory support.
The request moved slowly until Facility Engagement became active at the hospital, and newly-hired Project Manager Yuliya Zinova got to work to formalize meetings between the MSA and Interior Health. “This was when things started moving,” says Dr. Howatt. “Our interior Health partner understood the need, and the administrative support was provided by Facility Engagement.” FE Project Manager Yuliya Zinova arranged meetings with both physicians and the health authority administration, inquired about equipment to be funded by Interior Health, and arranged for funding physicians’ time spent training through Facility Engagement once the equipment was purchased.
“My precious commodity is time, and because of Yuliya’s help, we were able to take a good idea and turn it into reality,” noted Dr Howatt.
Peter Du Toit, Interior Health’s hospital administrator who sits on the Facility Engagement committee representing Interior Health said, “the discussions about the need for a CPAP system helped me better grasp the issue. FE helped speed-up the hospital’s purchase of the CPAP ventilator by at least three to six months.”
Facility Engagement is one of nine SSC initiatives that helps build relationships and assists in finding effective solutions for medical facilities across BC.

David Matear, Executive Director of IH West on Facility Engagement Initiative
Read More Read LessFor the Executive Director of IH West, David Matear, Facility Engagement and collaboration with the Chief of Staff, and the President and Vice President of the Royal Inland Hospital Physician Association (RIHPA) is helping solve a lot of issues facing the region.
David points out that one of the biggest challenges for the region has been minimal physician engagement at various levels, including involvement in decision making and understanding of the health authority’s strategies. “We need to realize that neither physicians nor administrators are successful as independent entities and they need to come together as collaborators to health system planning and delivery to ensure patients and families in our communities receive the highest quality of care.”
To further enhance this collaboration, Facility Engagement also provides learning opportunities where physicians and health authorities are able to work on joint projects to improve their facilities, something unprecedented in the history of BC health administration.
The joint leadership model (called Dyad) promoted by Facility Engagement is something that David really appreciates. “This model helps a great deal not only with creating partnerships and collaborative efforts, but also with enhancing the quality of the existing relationships by bringing out the best in people and utilizing those skills”. As an example, he referred to the process of “bringing together the physician leaders working on their projects and the IT leadership of the Interior Health to create a project inventory and provide strategic direction to support virtual care in IH West.”
David supports the work of Facility Engagement without hesitation, noting that “bringing physicians and administrative leaders to the same room sets the scene for a common understanding and is the beginning of a relationship.”
As of June 2018, there are 45 projects that are being supported by FE in IH West. Together with its partners, IH West went through an extensive process of strategic planning in January to set goals for the region, and involving physicians in those discussions. “This is huge. We are jointly discussing the goals for the next year. We’re basically on the same page, collectively, to facilitate health care delivery with a joint sense of responsibility.”
David concludes, “Even though we have a long way to go towards working together naturally and effortlessly, the realization that we no longer need to have separate conversations is a great lead into the future. While we move forward, it is important to keep reminding ourselves that the more collaborative our decision making, the more mature we become as a community of health care providers.”

Saving the Elk Valley Hospital Operating Room
Read More Read LessLittle did they know that the retirement of their only general surgeon at Elk Valley Hospital (EVH) in Fernie would bring about a significant opportunity for collaboration with both the physicians in the neighboring community and their Interior Health partner.
Having no luck with recruiting a new specialist surgeon for the hospital, despite a strong partnership with local governments to assist the recruitment efforts, physicians and staff started thinking about what could be done to save the OR. After all, this retirement could mean that surgical services in Elk Valley Hospital would have to close down and over 15,000 residents in Fernie, Elkford, Sparwood, Elko, and Jaffray would have to travel as much as 170 km to the nearest hospital in Cranbrook both for consultations and surgeries. Road conditions during the winter could make it even more challenging for patients to receive surgical care, especially for pregnant mothers requiring a C-section. Increased pressure on hospital staff and resources in Cranbrook from the additional elective day surgeries could also lead to longer wait times in that community.
In order to identify a solution that would save and sustain the OR in Fernie and not destabilize OR services in Cranbrook, physicians came together through funding from Facility Engagement to create a Surgical Sustainability Committee. The committee included representation from the physicians and Interior Health Authority (IHA) including the Chief of Staff, Health Services Administrator, Health Services Director, Site Manager, Medical Administrative Assistant, and Patient Care Coordinator (head nurse).
The solution conceived was both creative and sustainable, and involved the engagement of all parties. First, a Family Practitioner with Enhanced Surgical Skills (FPESS) was recruited to regain a slate of elective day surgeries in Fernie. However, as the FPESS was not starting for 12 months, the committee reached out to the Surgical Unit at East Kootenay Regional Hospital in Cranbrook, the neighboring city, to discuss an opportunity for them to perform surgeries at Elk Valley Hospital - with a goal of meeting patient needs closer to home while creating an opportunity to add sustainability to both surgical programs.
Through one-on-one personal phone calls made by committee members, specialist physicians in Cranbrook were able to discuss the opportunity and express their interest formally. EVH Physicians attended a Surgical Leadership meeting in Cranbrook to present the opportunity at their rural facility, and build their relationship with the Surgical Specialists.
Cranbrook surgeons were provided with all relevant information for working at Elk Valley Hospital, including the OR schedule of open days, an offer to have Fernie nurses travel to Cranbrook for a day to observe the surgeons’ working styles to build mutual comfort levels, and coverage of travel costs for surgeons through Northern and Isolation Assistance Outreach Program (NITAOP).In addition, an examination room was secured at Elk Valley Hospital for patient consults and equipped with furniture, donated local artwork, a fridge, and a nespresso machine to serve as a comfortable ‘home away from home’ for visiting surgeons as a model consultation space and a comfortable private space to take breaks between surgeries.
On the first day of work, Elk Valley Hospital staff and physicians came together for lunch sponsored by Facility Engagement to welcome and meet the visiting surgeons. Jacqueline Arling, the Facility Engagement Project Manager for Elk Valley Hospital, believes that the key to this solution was relationship building. “A big factor for the surgical sustainability success is that physicians have built trust and relationship with both the Cranbrook physicians and Interior Health.”
The residents of the Elk Valley now have four visiting general surgeons conducting consults and surgery at the Elk Valley Hospital, in addition to the current GPs and soon-to- start FPESS physician. The surgeons are proud of being able to help a neighboring community in need of specialist care. Taking collaboration to yet another level, these surgeons can also help mentor the local FPESS to expand their capabilities to perform surgeries in Fernie.
Reflecting on the success in Fernie, Karyn Morash, Health Services Director said, “With the advent of Divisions of Family Practice and Facility Engagement the way physicians were coming to the table was changing, it facilitated our ability to work more closely together.” while noting that “to the health authority’s credit, we have worked with determination to honor our part of the commitment to engagement with MSAs.”
Given the historical communication challenges that existed between health authorities and facility-based physicians, Elk Valley Hospital is a perfect case example of solution finding made possible through collaborative efforts leading in turn to improved patient care--the ultimate goal of the physicians, health authority and the Facility Engagement Initiative.

Facility Engagement in Interior Health: Dr. John Falconer
Read More Read LessWhen I think about where we started only a few years ago, I’m very excited ... Physician engagement among the groups continues to be excellent and growing. To me, one of the positive impacts has been the interdivisional and interdepartmental opportunities to regularly collaborate, such as pediatrics meeting with emergency or radiology meeting with surgery; these cross-collaborations are new. Read More >

Patient Simulation Expands at Kootenay Boundary
Read More Read LessPhoto credit: UBC Faculty of Medicine, Okanagan Campus
Facility Engagement is supporting medical staff from several departments at the Kootenay Boundary Regional Hospital in Trail to participate in the development of a simulation curriculum for different staff groups. One physician will work on ER based simulations, another will provide simulations for OR teams, and another will focus on providing "just in time," clinically-based simulations for critical care teams. After developing the curriculum, the physician lead for each area will also learn how to run the simulator, and provide educational sessions. The work will support local physicians and improve patient care.
-------------------
A perfect storm for patient simulation is generating new education and training opportunities at Kootenay Boundary Regional Hospital (KBRH) in Trail. As the acute care facility for Interior Health (IH) in the West Kootenay and Boundary region, the hospital supports a rural population of approximately 75,000 people. KBRH also serves as a primary learning environment for students with the Southern Medical Program (SMP) and resident physicians with UBC’s Kootenay Boundary family practice site.Dr. Scot Mountain, Director of the Intensive Care Unit, is one of the local physicians working closely with IH to develop a dedicated patient simulation centre for health professionals and learners.
Lillooet physicians work with partners to increase local mental health care access
Read More Read LessLike many rural and remote communities, Lillooet has struggled to provide appropriate local care for children and youth with mental health issues, particularly when they visit the Emergency Department and are then sent to the regional centre like Kamloops for psychiatric treatment.
Generally these are short-term solutions. Young patients return to the community with no follow-up available and often end up back at Emergency.
A solution was initiated by Dr. Humber and the Lillooet Hospital MSA physician group. The physicians worked together with local and regional Interior Health representatives, along with schools, First Nations councilors and other community members, to arrange for two Child and Youth Psychiatrists to provide outreach clinics to Lillooet and surrounding area.
With travel being a challenge even in the best weather, a blended model of face-to-face and virtual telemedicine was established, to enable physicians and patients to hold virtual follow-up appointments to reduce time between visits.
The value of the combined approach became evident when, during summer wildfires, road closures and nearby evaluations resulted in cancellations of the in-person outreach clinic. Patients were looking forward to their appointments, and thanks to the virtual telemedicine setup – and the collaborative process that made it possible – every patient was able to continue being seen by the psychiatrist.

Vernon physicians work to curb unnecessary repeated patient tests
Read More Read LessAt Vernon Jubilee Hospital, Dr. Jason Doyle brought forward concerns about redundant laboratory testing. Unnecessary, repeated rounds of tests for admitted hospital patients appeared to be occurring, and could potentially be preventable by modifying protocols.
The Vernon Jubilee Hospital Physician Society (VJHPS) arranged for a small representative group of physicians to examine laboratory utilization and develop recurrent laboratory testing guidelines for inpatients (such as guidelines for daily CBC orders).
They agreed on simple rules to govern, streamline and limit ordering of tests while patients are in hospital, and worked with the health authority to make changes to ordering practices at the unit clerk level. Through their Facility Engagement work, physicians had the opportunity to collaborate with the site and staff to implement the new guidelines.
As a result of the changes, we hope that patients will experience less anxiety and discomfort and will avoid unnecessary tests and that cost savings will be realized.
- Island Health

Preventing preterm births: physician-led initiative expands, save lives
Read More Read LessAn initiative created by two physicians on Vancouver Island is supporting maternity care providers to identify at-risk patients and use medical interventions to prevent preterm births. It can save lives and prevent devastating infant health issues, while helping families avoid the distress of travel to larger cities to access neonatal care.
Preterm births are the leading cause of perinatal mortality and morbidity in Canada and worldwide. Babies born before 37 weeks of gestation are at increased risk of severe and ongoing medical problems.Having a preterm baby is also stressful for parents, particularly those who live in smaller communities. Without access to specialized neo-natal intensive care, parents need to take time away from other children and jobs to seek care in bigger
 centres.
centres.Dr Jennifer Kask, a family physician attached to the Campbell River Maternity Clinic was aware of very high preterm birth rates in communities across Vancouver Island. Pre-term birth rates were as high as 25% among patients in 2016/17, compared to 7.4% and 7.8% in BC and Canada respectively (2013).
With the support of Facility Engagement funding, Dr Kask and Obstetrical specialist Dr Kirsten Duckitt set out to engage family physicians, midwives, and allied health providers in discussions about preventing pre-term births.
Simple intervention identified
They found that a simple vaginal progesterone intervention that helps at-risk patients extend their pregnancy to bring them closer to term was often used in specialist care by obstetricians, but not always by other providers or patients.
"We concluded there was a gap was in the knowledge of our colleagues and patients," says Dr Kask.
"We also knew a main risk factor for a mother having a preterm birth is having had a preterm birth previously," Dr Kask says. "So it was a matter of how we help to educate our colleagues and provide some resources to identify who is at risk, and how to help prevent recurrent preterm birth."
Creation of a pathway and resources for providers
Those insights led to their development of a Preterm Birth Pathway and education to help providers identify patients at risk, and use evidence-based, effective medical interventions to prevent preterm births. They created a package of resources including:
- a case-based CME event
- a care algorithm
- a clinician resource (a pre-printed Special Authority form developed through discussion with Pharmacare)
- patient education materials that included patient cards and posters
With education sessions and provider adoption underway in communities around Campbell River, Dr Kask then accessed SSC Spreading Quality Improvement Initiative funding expand the work more widely across Vancouver Island, including to Port Alberni and Tofino.
They also spread the education through the Cowichan Valley through direct work with the Cowichan Tribes. Dr. Kask notes that preterm births disproportionally affect First Nations individuals and created education resources to support those communities.
Results and next steps
Through data collected in her maternity clinic, Dr Kask notes there has been real progress in preventing preterm births, both through measurement in her clinic showing a downward trend in pre-term births, and patient experience stories.
Dr Kask and Duckitt continue to spread the work across Vancouver Island rural communities through 2023/24. She then hopes to further spread it across all BC regions, where providers and patients in smaller communities share the same experiences and risks, and can benefit from the pathway and interventions identified.
Dr Kask says that one of the highlights of the project has been making specialized care more accessible to other providers. “The neat part of it has really been the relationship and mentorship I’ve received from my colleague Dr Duckitt. She is an excellent educator, a wonderful OBGYN and was so willing to share her specialist knowledge.”
“When a patient delivers at term in their own community, and says, 'I am so grateful that I didn't have to go to an NICU this time.' it warms my heart. Particularly because it implies that they have a little person at home."
"I recognize that we are not going to able to prevent all preterm births, but recognizing that preterm birth is the biggest cause of perinatal morbidity and mortality, aren't all of them worth trying to prevent?" – Dr Jennier Kask
- PROVIDER RESOURCES: Pathway and patient posters
- WATCH: From Idea to Action to Spread: Dr. Jennifer Kask
- WATCH: Dr. Jennifer Kask: Raising Awareness on World Prematurity Day
This project has been funded by the Specialist Services Committee Facility Engagement and Spreading Quality Improvement initiatives. The Specialist Services Committee is one of four joint collaborative committees representing a partnership of Doctors of BC and the Government of BC.

ED simulation initiative 'undoubtedly saved lives' during the heat dome
Read More Read LessWhen the ‘heat dome’ descended recently onto British Columbia, many emergency departments were flooded with patients suffering from a dangerous condition known as hyperthermia. This rare but potentially life-threatening condition is not frequently seen in the emergency room, yet requires specialized, time-sensitive treatment.
 Fortunately, Victoria-based Emergency Department (ED) physicians had run a hyperthermia scenario a year prior through its ED Simulation initiative, and identified important gaps in care that could be remediated.
Fortunately, Victoria-based Emergency Department (ED) physicians had run a hyperthermia scenario a year prior through its ED Simulation initiative, and identified important gaps in care that could be remediated.These included having ready access to cooled-IV fluids, body bags that could be filled with ice and water to further cool patients, and fans for misting.
On the eve of the 2021 surge in temperatures, these lessons learned were recirculated to Victoria Emergency Departments so that all staff could be as prepared as possible.
Over the next few days, patients flooded the Emergency Departments of both the Victoria General and Royal Jubilee hospitals.
"Our team functioned on the brink of crisis/Code Orange due to the sheer volume of high acuity patients. Fortunately, our team had run heatstroke and mass casualty simulations in the past. This undoubtedly saved lives”. - Dr. Jacob Wilkins, Victoria General Hospital.
Another physician remarked that the previous simulation was referenced a number of times by staff during the heat wave episode, and that the ED was stocked with supplies that they don’t normally carry. “Once again”, this clinician concluded, “a patient has benefitted from this program."
"I spent my entire shift resuscitating a steady stream of Hyperthermic patients. At one point, I had three comatose patients with core temperatures above 40C, and who were also hemodynamically unstable, arrive all at the same time.
Nevertheless, I felt strikingly ready for the challenge as, by chance, one of our recent Simulation Sessions in the Emergency Department was based on just such an event. When we began to hear that a heat wave was being forecast, it allowed us to review the case as a group and discuss the pearls of wisdom gleaned from it.
Our critical care colleagues were able to add to our knowledge as we shared our post-simulation discussion electronically and department wide. Thus, when patients began arriving incessantly, there was no need to review treatments or cognitively think through work-arounds as problems arose. I could simply act. And, in doing so, I truly believe we were able to save lives that night that perhaps would have been otherwise lost." - Dr. Matt Bouchard
Thank you to Dr. Matt Carere, Dr. Donovan MacDonald, and their colleagues in the Emergency Department and other participating departments, for this life-saving initiative!
In situ simulations continue to show benefits
This is not the first time a patient has received excellent care on the heels of a simulation exercise. For the past several years, Victoria-based Emergency Department physicians have been running in situ simulation exercises in collaboration with colleagues from other departments.
Funded by the South Island Medical Staff Association through the Facility Engagement Initiative, these simulations have promoted a culture of learning, interaction and continuous improvement.
Of particular interest has been simulating cases of HALO events - High Acuity, Low Occurrence. As the name suggests, these happen infrequently but require precise, time-sensitive responses when they do occur.
The heat dome crisis further reinforces the value of regularly simulating HALO events with a multidisciplinary team. The benefits for clinician and staff morale, team building, and most importantly patient care, continue to emerge.
Other recent simulations run through the Victoria In Situ Simulation Program include: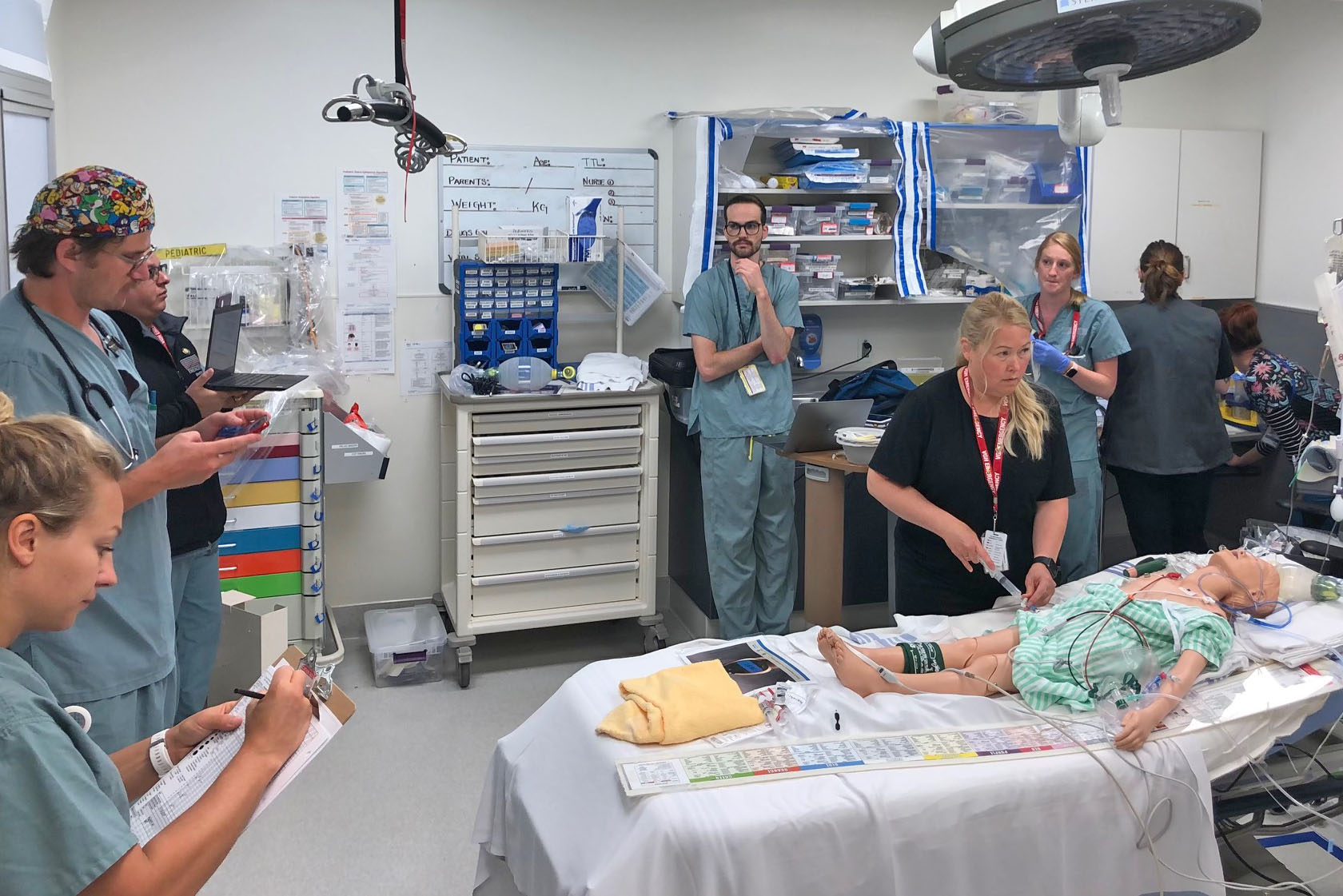 Sympathomimetic overdose with hyperthermia (ED, Nursing, RTs, Lab techs, XRAY, unit aides)
Sympathomimetic overdose with hyperthermia (ED, Nursing, RTs, Lab techs, XRAY, unit aides)
- Beta-blocker overdose + COVID AGMP practice (ED, ICU, Nursing, RT, SIM lab support)
- Precipitous delivery, post partum hemorrhage (ED, OB/GYN, LDR nursing, ER nursing, unit aides)
- COVID sudden cardiac arrest in the department (ED, ICU, Nursing, RT, Sim lab support, Unit aide)
- Pediatric trauma, intracranial injury, hemorrhagic shock (ED, PICU, Nursing, RT, labs, Diagnostic imaging, Unit aide)
- Pregnant female with Iron overdose (ED, ICU, Nursing, RT, Unit Aide, Unit Clerks)
- 22 year old COVID positive patient with cardiomyopathy and cardiogenic shock (ED, Trauma, Nursing, RT, Unit Aide, Unit Clerks)
- Breech delivery at the Jubilee requiring NRP (ED, OB/GYN, Nursing, Unit Aide, Unit Clerks, Midwife)
- Trauma, facial burns, airway case and cyanide toxicity (ED, Intensivist, Nursing, RT, Unit Aides)

Campbell River Spirit Awards 2020 – Recognizing Inspiration and Dedication
Read More Read LessTo say 2020 has been challenging, particularly for anyone who worked in health care would be the greatest of understatements. The Campbell River Spirit Awards is a way of honouring a few of the many people who continue to keep the Campbell River community healthy.
The Spirit Awards are the result of a joint collaboration between the Campbell River and District Division of Family Practice and the Campbell River Medical Staff Engagement Initiative. The initial idea came from Dr. Ninette Fourie who is involved in the Doctors of BC Physician Wellness Program and the Division of Family Practice.
Dr Fourie says, “Burnout can be prevented by fostering a culture of appreciation and mutual respect that in turn supports resilience, balance and meaning. We wanted to create a high profile event to showcase the silent sacrifices made by our local physicians and their families.”
Understanding the importance of recognition in helping to maintain physician wellness, the Spirit Awards began its journey. Drs Fourie and Marissa Dry formed and participated in a planning committee, which included determining recognition categories, promoting the awards and soliciting nominations.
Almost all physicians in the community have hospital privileges and Campbell Rivers’ new hospital has a very active doctor’s lounge that is well-used by physicians, so it was easy to promote the awards and get engagement. The physicians could make their nominations using a paper ballot or through an electronic portal.
To celebrate, a video captured the virtual event, which included comedy, musical guests and many heart-felt words. Co-hosted by Drs Victor Jordan and Natasha Rafo, the common themes expressed by all award recipients were the value of teamwork, the luxury of having inspiring and giving colleagues, and the rewarding nature of providing health care in a small community.
The awards also honoured non-physicians, presenting the Community Advocacy and Integrity Award to Christine Colbert, Executive Director, Campbell River and District Division of Family Practice, and to The Foundry (John Howard Society North Island).
The awards given to a number of deserving physicians are as follows:
SUPERHERO AWARD
Dr Erika Kellerhals, a family physician who works hard to reduce the stigma of mental health, poverty and addiction, particularly in marginalized communities and Dr Kirsten Duckitt, an OB/GYN who in addition to taking care of patients, tirelessly participates in a number of committees formed to help improve the work environment for physicians and health care for patients.
PHYSICIAN LEADERSHIP
Dr Jennifer Grace an internist who really stepped-up and took an active leadership role to help manage the delivery of health care during the unprecedented pandemic.
RURAL AND REMOTE CHAMPION
Dr Ellen Anderson, a family physician who provides a full-service practice to the Cortez Island community, which was particularly challenging during 2020.
EXCELLENCE IN PATIENT CARE
Dr Robert Ramsey, a family physician and internist Dr Aadil Dhansay have both been described as the ones you call in the middle of the night – they are always there with their expertise and wisdom.
INNOVATIONS IN PATIENT CARE
Dr Jennifer Kask, a family practice physician, and Dr Leanne Wood, a general surgeon have both contributed greatly to improvement to patient care and access to health care services. Through numerous patient center quality improvement projects. Dr Kask has ensured a high level of maternity care for families throughout the North Island with her leadership in the development of the Maternity Clinic in the Campbell River Hospital. Through her early development of educational and instructional materials and videos to support GPs in rural settings, her forward thinking process has reduced the need for in-office visits during the pandemic.
Dr Leanne Wood was a key lead in the Enhanced Recovery after Surgery program and has gone on to be the specialist lead in the Surgical Patient Optimization Collaborative, both focused on early supports for patients to experience more positive post-operative outcomes. She also continues to bring breast cancer surgery closer to home.
EXCELLENCE IN PARTNERSHIP
Dr Angela Logan, a family physician who has worked on multiple committees to help improve patient and community care with the belief that building trust and mutual respect results in improvements for everyone.
EXCELLENCE IN EDUCATION AND COMPETENCY
Dr Natasha Rafo, a family physician who helped establish the simulation centre at the Campbell River Hospital to further the medical education of physicians through hands-on, simulated learning.
LIFETIME ACHIEVEMENT AWARD
Dr. Larry Ness, a long-serving family physician within the community who exemplified compassion and kindness through-out his career. Through the years, Dr Ness has also participated in a many humanitarian missions in various countries.
The inaugural Campbell River Spirit Awards was a great success, and all the award recipients verbalized their appreciation for their colleagues. The Spirit Awards Committee created the opportunity, but it was talented co-hosts, musical guests, the winners and participants that generated the laughter and the tears.
It is hoped that at the next award season this event will be a face-to-face gathering that really delivers the true spirit of celebration and community.


Shifting paradigms
Read More Read LessAs a family physician working in a maternity clinic in Comox, Dr Theresa Wilson observes families interacting with each other and sometimes witnesses the frustrations related to adapting to a child’s development. This is an experience not unfamiliar to her during some of her visits with families with young children.
“All parents want to do well by their child, and all parents have strengths,” says Dr Wilson, who credits Touchpoints for her understanding that relationships are the foundation for development.
Dr Wilson first learned about Touchpoints and attended the initial training when it was brought to the Comox Valley by the Pathways to Healing Partnership and a public health nursing coordinator.
Touchpoints is a framework that guides practitioners to intentionally build on relationships between physicians and parents and their families, and between parents and their young children.
Dr Wilson explains that using the Touchpoints guiding principles is a culturally responsive approach to care as it can help practitioners recognize and understand the differences of patients before and during a visit –meeting patients where they are at. Physicians can use the child’s behavior to learn more about where the family is at, and how they are coping with a new developmental change or challenge. The Touchpoints principles also helps physicians observe interactions for strengths.
“You’re doing what you’re doing, just better. We are genuinely changing how we see people by becoming more self-aware,” says Dr Wilson.
Physicians can shift conversations between parents and children from what is not working to what is working well. Through reflection and practice, physicians work alongside families during predictable periods of disorganization or regression as a child learns or acquires a new skill or milestone.
“I can help parents to see that it’s okay that their child's development fluctuates when the child is working on a learning a new skill,” says Dr Wilson. “I can help normalize the ups-and-down.”
Strengthening the parent-child relationship
Dr Wilson recalls a time when she was with a patient who had just delivered her child. The patient’s partner had rushed into the patient room, missing the birth by eight minutes. Recognizing that the father was disappointed, Dr Wilson was able to help reframe the experience.
“I had seen the baby turn its head to look at the father when he came into the room,” shares Dr Wilson. “So I pointed that out to the father, who hadn’t seen it. I was able to use the language of the baby and narrate its behavior.”
By focusing on the positive aspects of the situation, Dr Wilson transformed how the interaction was remembered by the family.
Reducing physician burnout
By using the Touchpoints approach with patients, doctors can help reduce their own stress and feelings of burnout.
Before a patient visit, Dr Wilson reviews the area of development, looking for what might be seen or expected during the visit and reflecting on potential Touchpoints assumptions and guidelines. With that preparation, she feels grounded and ready for difficult issues that may come up during the interaction.
“My patients have commented about how they appreciate the extra time I’m spending with them, but that’s not the case,” says Dr Wilson. “My visit times have not changed.”
In 2018, Dr Wilson became a registered Touchpoints trainer in BC with the support of the Shared Care Committee (SSC) and Comox Valley Division of Family Practice.
Supported by the Physician Engagement Society of Comox and Courtney, which is funded by the Facility Engagement Initiative, the interactive training is offered to doctors through the Comox Valley Child Development Association (CVCDA). For more information, contact the CVCDA.
Watch the video below to learn more about Touchpoints from a panel of multidisciplinary health practitioners in BC.
The webinar is presented by the Shared Care Committee –one of four Joint Collaborative Committees that represent a partnership of Doctors of BC and BC Government– and the CVCDA.

Simulating emergencies bring invaluable results
Read More Read Less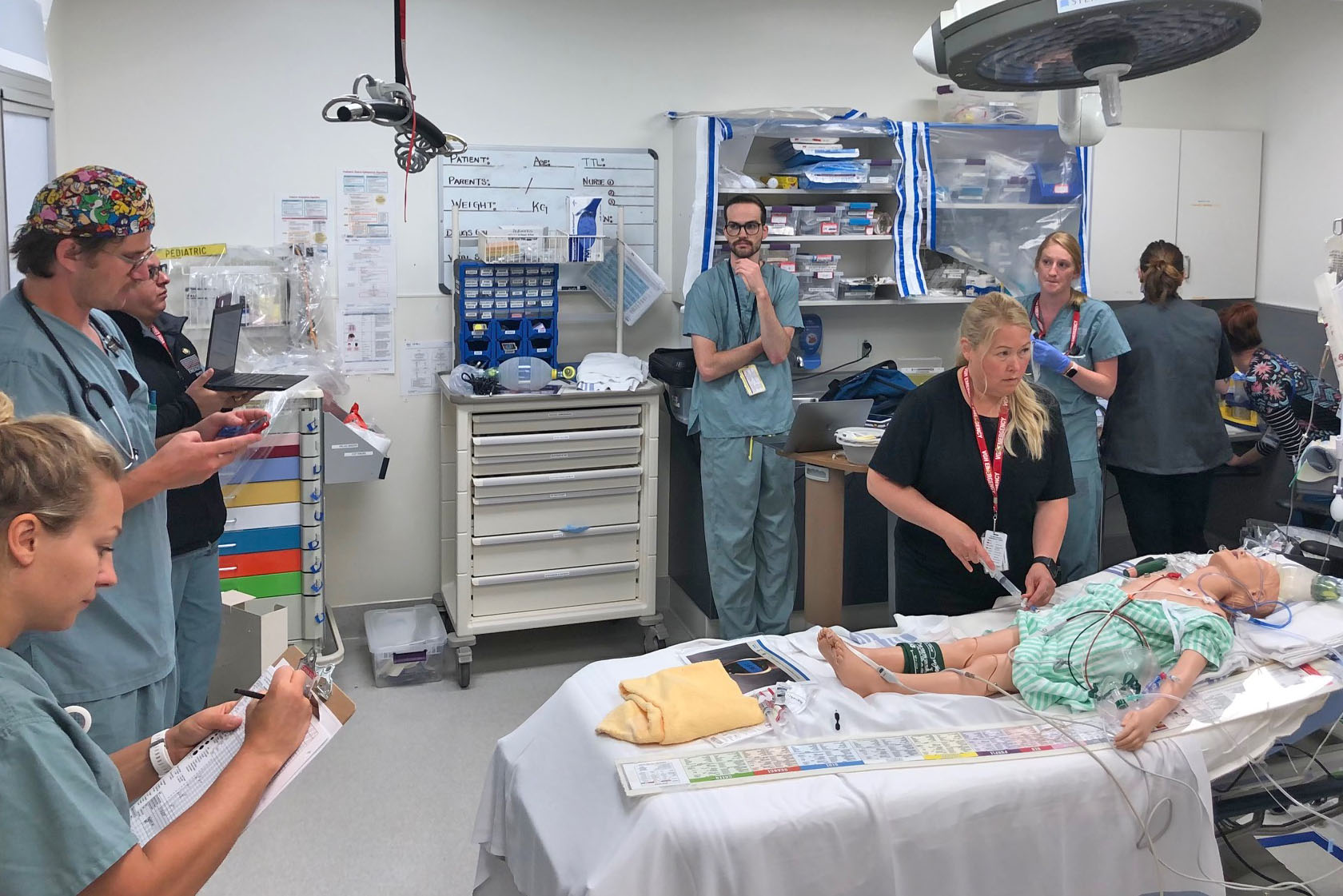
Any hospital’s Emergency Department (ED) has seen life-threatening drama and life-saving results – often it is preparation that makes the difference. Dr Matt Carere, an ED doctor at the Victoria General Hospital knows well the importance of being prepared.
During the past year or so, he along with Dr Donovan MacDonald, an emergency medicine resident doing a Fellowship in simulation training, with the support of ED Department Heads Drs Paul Collela and Gavin Jones, and help from the South Island Medical Staff Association's Facility Engagement Initiative funding have brought “in situ simulation” training to the hospital’s ED.
This training allows ED staff and relevant specialties to work, learn and reinforce their skills together in their clinical environment. It also helps identify hazards and deficiencies within clinical systems, the environment and the health team. This is unlike the traditional simulation training conducted at teaching hospitals.
From simulation to real life
A recent in situ simulation helped save the life of a two-week old newborn. Dr Carere, “there is nothing more daunting than having a two-week old premature baby in profound shock and peri-arrest come in. And nothing more satisfying than being able to work in the most efficient way possible to save her because we had just run a simulation a week previously that yielded a number of critical changes to our approach.”
Over the last year, one to two simulations were held each month, involving not only Emergency Department physicians, but also Pediatric Intensive Care docs, PICU and NICU nurses, pediatricians, hematopathologists, anesthesiologists, adult intensivists, respiratory therapists, ECG and lab technicians, as well as more than 40 different emergency department nurses.
Dr Carere notes, “getting them to come in and give us their input on how we can improve our practices in the ED is invaluable. This doesn’t happen without complete buy in from everyone. In fact, we have a group of nurses who volunteer for these nursing education days. They’re getting examined under a microscope by us and they are all for it.”
“There is nothing more daunting than having a two-week old premature baby in profound shock and peri-arrest come in. And nothing more satisfying than being able to work in the most efficient way possible to save her because we had just run a simulation a week previously that yielded a number of critical changes to our approach.
A learning opportunity
Each scenario is attended by a clinical nurse educator to summarize the scenario and lessons learned to ensure any insights or needed actions are given to all ED staff. The group also film each simulation so that those not able to attend on the day can still learn from the experience. Dr Carere states, “It’s humbling because I’m in these rooms with all these talented doctors and nurses and every time I personally am learning so much.”
Due to COVID, some practices have been made more complicated. With in situ simulations, even the smallest barriers can be revealed to have a huge impact. For example, a recent simulation involved a cardiac arrest with a suspected COVID patient. One doctor discovered administering CPR in full PPE with glasses, googles and face mask left him unable to see as his glasses continually fogged up.
The South Island Medical Staff Association's FEI funding funding has been inestimable in allowing this work to happen. Feedback has been universally positive from staff to the hospital administration. Dr Carere is working to help make in situ simulation become a natural part of the hospital’s culture.

Cultural Connections: Collaborating for Healing in Health Care
Read More Read Less
In early 2020, Tla-o-qui-aht First Nation community members led a group of Tofino health care professionals through a cultural ceremony where they experienced traditional healing practices first-hand. Together, they wanted to explore how these practices and stronger cultural connections might blend with medical care to support people who experience trauma and pain.
Tla-o-qui-aht First Nation healer Nora Martin and cultural worker Chris Seitcher led the ceremony, which included Tla-o-qui-aht members, physicians, nurses, X-ray and laboratory technicians, and a firefighter.
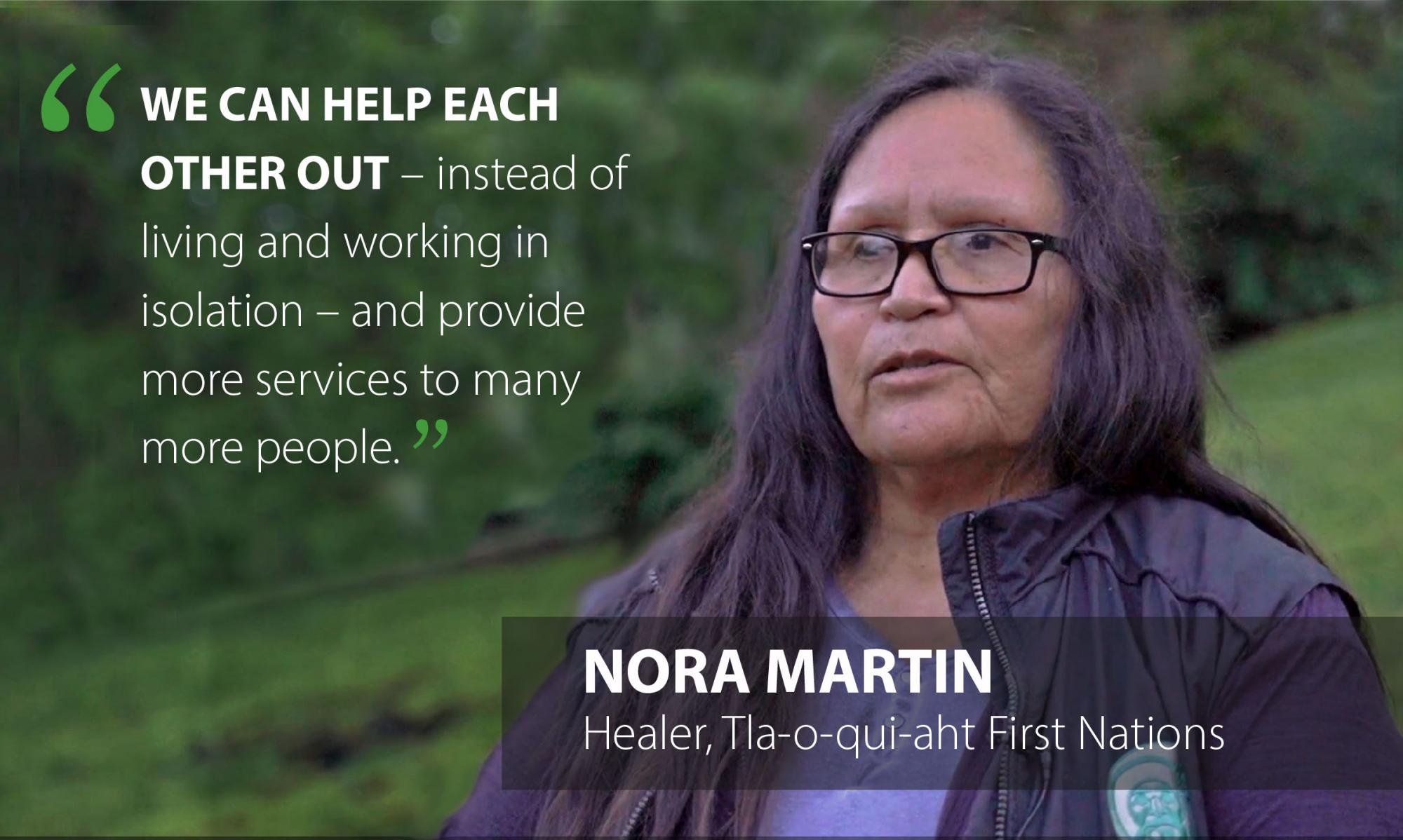 Martin explains that traditional cleansing ceremonies have been used by her ancestors for generations and continue today. “We carry trauma around with us, and sometimes never deal with it,” she explains. “In our community, if there is a serious incident or death, we do these kinds of ceremonies for community members right away. It makes a big difference.”
Martin explains that traditional cleansing ceremonies have been used by her ancestors for generations and continue today. “We carry trauma around with us, and sometimes never deal with it,” she explains. “In our community, if there is a serious incident or death, we do these kinds of ceremonies for community members right away. It makes a big difference.”Those benefits caught the attention of Tofino primary care and emergency room physician Dr. Luke Williston. He had seen for himself how traditional cultural practices helped a group of patients who were struggling to deal with trauma and experiencing substance use that required frequent treatment in hospital.
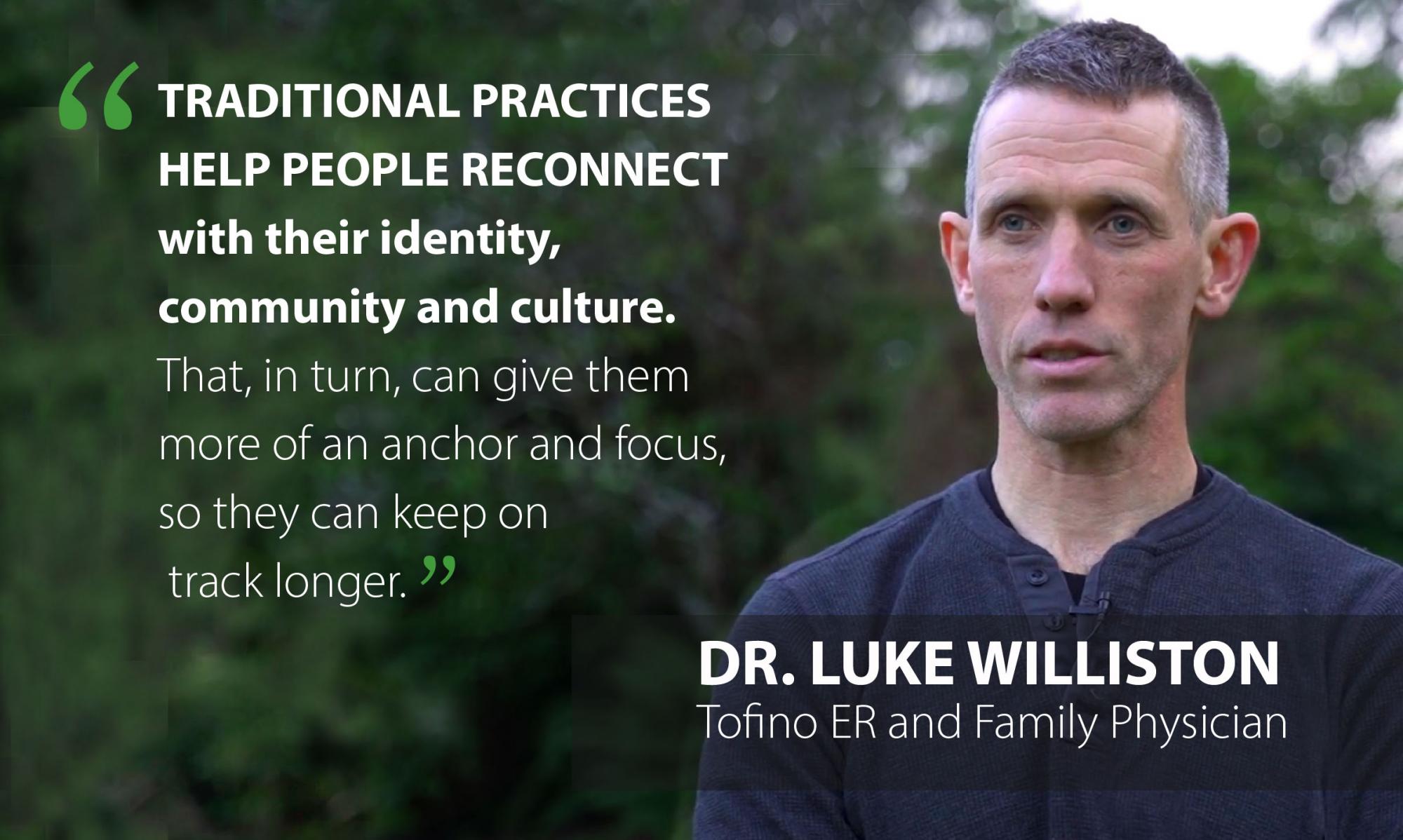 “A First Nations cultural worker came to the hospital to do a cleansing ceremony for some patients,” he says. “We didn’t see any of those patients for more than a year after. When I would see them in the community, I could see they were doing better. That is hard to ignore."
“A First Nations cultural worker came to the hospital to do a cleansing ceremony for some patients,” he says. “We didn’t see any of those patients for more than a year after. When I would see them in the community, I could see they were doing better. That is hard to ignore."“While our current medical therapies are good, they do not always hit true with everyone.”
He observes that traditional practices help people reconnect with their identity, community and culture. “That, in turn, can give them more of an anchor and focus, so they can keep on track longer.”
VISION FOR A HEALING COMMUNITY
Williston wanted to learn more. With funding from Facility Engagement and the Rural and Remote Division of Family Practice, he connected with Martin and Seitcher to explore how they could work together to introduce health care colleagues to traditional practices, and over time, create a more connected healing community. Chris Seitcher has worked in the helping field for many years, including as a care aid with Island Health, and for elders in the Tla-o-qui-aht Nation. He runs a weekly men’s group, which he describes as being a supportive, safe space for community members to share stories, history, traumas, and emotions. Traditional chanting and singing are also incorporated to help change the energy.
Chris Seitcher has worked in the helping field for many years, including as a care aid with Island Health, and for elders in the Tla-o-qui-aht Nation. He runs a weekly men’s group, which he describes as being a supportive, safe space for community members to share stories, history, traumas, and emotions. Traditional chanting and singing are also incorporated to help change the energy. “This is how we deal with our trauma, our suffering, our pain,” he explains. “When we have safe space and support where we can share things that are happening inside—things we don’t usually talk about—then things start to slowly change.”
Williston feels that health care workers can also benefit from some of these approaches. “We get exposed to a lot of trauma at the hospital all day,” he says. “We all need to find healing for ourselves.”
EXPLORING THE OPPORTUNITY TOGETHER
 A collaborative plan unfolded. Martin and Seitcher arranged to hold a traditional cultural ceremony that was recorded on video. It incorporated a talking circle, breathing exercises, and drumming and singing led by Hayden Seitcher, also of the Tla-o-qui-aht First Nation.
A collaborative plan unfolded. Martin and Seitcher arranged to hold a traditional cultural ceremony that was recorded on video. It incorporated a talking circle, breathing exercises, and drumming and singing led by Hayden Seitcher, also of the Tla-o-qui-aht First Nation.Pools were set up at Načiks (Clayoquot Heritage Museum at Monks Point in Tofino) for the group to experience cold water cleansing.
“Any time there was trauma in the community, or family, grief, or loss, we would bring members to the river or ocean to do a cleansing,” explains Martin. “Cold water rebalances us: it refocuses negative energy…to help clear the mind.”
The ceremony was an insightful learning experience for the guests. “It is quite different from our usual kind of medical work—a much slower pace,” says participant Dr. Pam Frazee. “A different part of your brain is working—your emotions are more present.”
STRENGTHENING CULTURAL CONNECTIONS
 Over time, the aim of those involved is to introduce traditional healing practices more widely with health care professionals, ambulance crews, firefighters, the coast guard, and police officers—all of whom are exposed to emotional and physical trauma—and to create stronger cultural connections among patients, health care, and emergency professionals.
Over time, the aim of those involved is to introduce traditional healing practices more widely with health care professionals, ambulance crews, firefighters, the coast guard, and police officers—all of whom are exposed to emotional and physical trauma—and to create stronger cultural connections among patients, health care, and emergency professionals.“These providers work in First Nations communities and may not have that connection yet,” says Williston, who sees benefits of making traditional, non-medical interventions more available to health professionals. He suggests that paramedics, for example, could introduce some of the techniques that help reduce a patient’s anxiety before getting to the hospital.
Additionally, cultural workers could be integrated into the hospital to perform ceremonies for sick patients and those who are soon to be discharged. “That surrounding care might help [patients] stay better, longer,” says Williston.
 Seitcher also sees many benefits to blending in traditional practices. “Culture is always around us,” he says. “Culture means connection. We can bring our culture to the hospital and create a safe space to connect and work through some tough issues.”
Seitcher also sees many benefits to blending in traditional practices. “Culture is always around us,” he says. “Culture means connection. We can bring our culture to the hospital and create a safe space to connect and work through some tough issues.”
Martin, reflecting on her first time working with the medical community, says she is pleased to see the openness to new ways and new learning.It supports an aim of the First Nations Health Authority and BC’s health care system to have First Nations communities and members work in partnership with doctors and health care professionals to support people’s health, wellness and care.
“We have a lot to offer,” she says. “We can help each other out – instead of living and working in isolation – and provide more services to many more people.”
Watch: Traditional Cleansing Ceremony>
This project was supported by Facility Engagement, a Specialist Services Committee (SSC) Initiative, and the Rural and Remote Division of Family Practice, an Initiative of the General Practice Services Committee (GPSC). The SSC and GPSC are Joint Collaborative Committees of the Government of BC and Doctors of BC.

Physicians Lead the Way to Hospital at Home
Read More Read LessVictoria-area physicians have engaged providers and partners from across the hospital, region, and at government levels to introduce a new model of care for Hospital at Home to BC.
Victoria Hospitalists Dr. Elisabeth Crisci and Dr. Shauna Tierney have been unwavering in their pursuit of a new kind of care for patients. Now, their passion project is about to become a reality with the BC Government’s launch of Hospital at Home across the province.
With Hospital at Home (HaH), acutely ill adult patients who are at lower risk and have a predictable clinical path can get hospital-level care from a team of professionals at home, safely and effectively. The model has been used for years in countries like Australia and the UK.
Extensive studies, including three Cochrane reviews (Ref 1), show that HaH provides equivalent or better clinical outcomes than standard hospitalization. Length of stay tends to be shorter and there is a higher level of satisfaction amongst patients, their caregivers and healthcare workers. It also shields patients from some of the complications associated with a brick and mortar hospital stay.
Dr. Crisci first saw HaH in action several years ago while doing fellowship training in Australia. “This was not home and community care. It was acute, hospital-level care: IV medications, blood transfusions, oxygen. There is no doubt in my mind that those patients, if they were back in Canada, would need to be on a hospital ward.”
“A hospital is an unsettling environment, especially for frail and elderly patients,” she says. “I thought, ‘why can’t we do the same in Canada?’ The expertise and therapies that we associate with hospital care are all portable, and so is the hospital staff.”
“It is an opportunity to offer safer, more patient-centered care for our patients and for less cost. It is the right thing to do.”
Back in Canada, she often thought about the HaH model. Then, in 2019, an opportunity came up to take action. Her Hospitalist colleague, Dr. Shauna Tierney, was reading about a HaH program for COPD and was inspired.
“I saw that we could do better for our patients’ dignity and comfort, and thought, “we have a moral imperative to do this." - Dr. Shauna Tierney
Dr. Tierney reached out to Island Health and her Hospitalist colleagues to see what could be done. Dr. Crisci was ready. “We knew that we needed to join forces to make this happen.”

Left: Dr Elisabeth Crisci. Right: Dr Shauna Tierney
Collaboration moves the vision forward
The two physicians would need help to develop a HaH program for BC– including the buy-in and support of the Island Health, South Island Hospitalists, the Divisions of Family Practice, and eventually, the Ministry of Health. Funding from Health System Redesign and Facility Engagement made that possible.
“Over the past year we worked relentlessly to get the level of engagement this project requires, while developing our own HaH program for B.C.” says Dr. Tierney. It meant that they had to become agents of change, inspire others to think outside of the box, and challenge some old-standing beliefs about how hospital-care can be delivered.
“The same old thinking will always give you the same old results,” says Dr. Crisci. “We argue that what should define hospital-level or acute-care is the type of patient and the type of clinical interventions required, rather that adhering to a definition based on the physical location of the patient.”
Taking the hospital team and interventions to the patient's home would require further support, which they sought from the BC Ministry of Health. “We don’t want this to be just another community-based service,” says Dr. Crisci.
“We want a true substitute to a standard hospital admission. For this to be possible, we have to ensure that these patients fall under the governance of the provincial Hospital Act. This means that even if at home, these patients are admitted and under the responsibility of the hospital.”
To their delight, the Ministry was interested in doing much more with HaH, and in September 2020, announced that BC would introduce the model to Victoria, and then spread it across the province. In part, HaH can help with the government’s COVID-19 planning by freeing up some acute care capacity.
Next steps
While there are details to iron out to pilot HaH at Victoria General Hospital and eventually scale to other hospitals, a full-time project team is in place to take the work over the finish line. The doctors are continuing as medical leads.
They note that experienced physicians on the ground are uniquely positioned to bring innovative ideas such as this to the fore. But they could not have done it alone. It took everyone’s help to make their vision a reality.
“It has been quite an adventure. It started with two physicians with an idea, and now HaH is one of the priorities for BC’s health care system,” says Dr. Tierney.
“The collaborative effort between the Ministry, Island Health and the front-line physicians has been incredible; something I never thought I’d ever witness in my career,” agrees Dr. Crisci. “Here we are, side-by-side, to not only improve the care of patients but also working to make our system a bit more sustainable.”
"I can’t wait to see that first patient’s face when I can say, “you get to go home, and I will come to see you at home.” - Dr. Elisabeth Crisci
Funding for physician engagement in the HaH project was provided by Health System Redesign (HSR), an initiative of the Joint Collaborative Committees (JCCs) representing a partnership of Doctors of BC and the Government of BC – and the South Island Medical Staff Association, funded through the South Island Facility Engagement Society and Specialist Services Committee, one of the four Joint Collaborative Committees.Ref 1: Cochrane Reviews
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD007491.pub2/full
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000356.pub4/full

Collaboration produces COVID-19 patient care tool in 10 days
Read More Read LessROYAL JUBILEE AND VICTORIA GENERAL HOSPITALS, SOUTH ISLAND: In pandemic planning, having a source of truth and standardized approaches are essential to coordinated and efficient responses. So is speed. In March 2020, physicians from the South Island worked together with colleagues, Island Health administrators, staff, and allied health providers to develop a COVID-19 Clinical Order Set in just 10 days.
Clinical order sets serve as a common platform for decisions made at the point of care. They compile the best evidence and best practice in one place to reduce variation in practice, and ensure patient safety.
South Island Hospitalists Dr David Cook and Dr Jean Maskey had already been working alongside a Clinical Order Set Harmonization Team to update clinical order sets (COS) to align with current evidence and harmonize with the future roll-out of iHealth.
With joint project funding from Facility Engagement and Health System Redesign, they planned to reach out to hospitalists, community family physicians and various hospital specialists for input.But they didn’t expect to have their processes and relationships tested by the outbreak of the novel SARS-CoV-2.
Quickly pivoting, they drafted a new COVID-19 clinical order set based on current knowledge about treating patients with the virus. Its development required bringing together a group of agile, efficient and dedicated medical staff and administrators – a process tirelessly organized by Alison Steinbart, Medication Safety Consultant.
Within 10 days – by the end of March 2020 – the order set was ready to go, with much appreciation from front-line staff caring for these patients.
The rapid development of the COVID-19 Clinical Order Set by the Island Health team drew attention at provincial tables, where there was interest in scaling up the work and sharing it with other health partners.“This was a BIG success for the team to complete this order set from start to finish so quickly, especially in this unprecedented time of increased anxiety, social isolation and new workflows in anticipation of patients with this new and potentially life-threatening condition,” said Dr Maskey.
Good thing we had established solid relationships between clinicians and the Order Set Team, due to our work done together over the past year, giving us both practice working with each other, and knowledge of the format and process, as that really helped!”
— Dr Jean Maskey, Co-lead, South Island HospitalistThe project leads realized the value of collaborating widely with practicing physicians to improve both acceptance of the order set by clinicians, and excellence in care by incorporating current evidence-based practices.
They also recognized the challenge of having a large group of physicians participate in these processes, and saw Facility Engagement funding as instrumental to its success.
The team performed these updates so effectively that Dr Cook was asked by the Clinical Order Set Harmonization Team to extend his work as a physician champion of order sets in an ongoing basis.One of the gratifying things we witnessed during the pandemic was medical and non-medical staff coming together with a sense of urgency to contribute to important work integral to Island Health’s operational response to the pandemic. The work on the COVID-19 Clinical Order Set is a prime example of this.”
— Dr Ian Thompson, Acting Chief Medical Officer, Executive Medical Director, Medical Staff Governance Medical & Academic Affairs, Island HealthWHO WAS ENGAGED?
- Physicians
- Order Set Team
- Administrators
- Island Health Informatics team
Specialty Areas
- Infectious Disease
- Internal Medicine
- Hospitalists
- Emergency
- Lab Medicine
- Intensive Care Unit
- Pharmacy
- Palliative
- Primary Care
- Respirology
There were many more people giving input than the folks listed – I think everyone should get a shout out for giving time when they were quite busy.”
— Dr David Cook, Co-lead South Island HospitalistRead the full story at www.southislandmsa.ca and Island Health Medical Staff website.

Vancouver Island physicians "Where I work, live and care"
Read More Read LessDr. Bruce Campana, Dr. Omar Ahmad and the South Island Medical Staff Association have launched "We Are Island Health" - an inside look at what matters to medical professionals from Victoria to Tofino and Port Hardy, and what makes their work special.
Take a look here!
Telemetry Unit changes improve patient flow, care and reduce wait times
Read More Read Less
The Comox Valley Hospital Telemetry Unit is an eight-bed unit caring for cardiac and high acuity patients. Before December 2020, any hospital physician was able to admit patients to this unit leading to variability in admission criteria, reduced patient flow, and challenges with multidisciplinary communication. Sometimes, stable patients who were ready for the ward would remain in the Telemetry Unit while other patients with heart attacks were held in the Emergency Department (ED). But that changed when Dr. Samuel Kohen’s physician-led initiative helped to reduce the time patients wait to be transferred from the ED to the Telemetry Unit by 52%.
Drawing on critical care and cardiology literature, Dr. Sam Kohen, an Internal Medicine and Critical Care specialist, believed that patients would receive more appropriate and timely care by transitioning the Telemetry Unit to a “closed” model of care, where only Internal Medicine physicians could admit patients.
Dr. Kohen has a Master’s in Quality Improvement and Patient Safety, completed the Sauder Physician Leadership Program and was an Island Health Physician Quality Improvement (PQI) advisor.
To test this idea, Dr. Kohen started by getting support and Facility Engagement funding from the Physician Engagement Society of Comox and Courtenay (PESCCI). Dr. Kohen notes, “with the funding I received from the medical staff association, I was able to hire Dr. Madalene Earp (PhD) to help with research support, and PESCCI helped me gain access to key stakeholders within the hospital administration.”
The primary aim of the Telemetry Optimization Project was to reduce the time patients wait to be transferred from the Emergency Department to the Telemetry Unit by 50%. Other measures of interest included hospital and telemetry unit length of stay, 30-day mortality, multi-disciplinary communication, and health care provider satisfaction.
To reliably measure the effect of “closing” the Telemetry Unit, Dr. Kohen collected one year of retrospective data and administered a pre-transition provider engagement survey to gather stakeholders’ opinions and support for the proposed transition. Unit operations transitioned in late 2019 after which Dr. Kohen collected one year of prospective data. In the end, the operational changes decreased the time Telemetry patients waited in the emergency department from a median of 6.7 down to 3.2 hours, a 52% reduction.
A key component of this project was data management, Dr. Kohen said, “The research support was incredibly valuable. Madalene liaised with health authority database administrators, aggregated the data, performed appropriate statistical analyses, and helped me write the reports. Frankly, she is better, faster and more cost effective than me at managing most research processes – and without her, I don’t think I could have completed this project while maintaining my clinical practice and personal life.”
The work also served to identify some areas for further improvement in the unit including increased staffing and educational support.
Dr. Kohen is now considering a follow-up project to further improve hospital-wide critical care patient flow. He believes, “If we all work together and focus on quality, we can affect great system improvement – and make sure that all patients receive the type of care we would want for our loved ones.”

Heart Health Team aims to improve AED data sharing
Read More Read LessWhen a person experiences cardiac arrest, paramedics and first responders may use an Automated External Defibrillator to help “re-set” the heart rhythm. Not all cardiac arrests receive a shock, but all AEDs collect important heart rhythm and rate data that can help the Heart Health team determine what caused the heart to stop and guide treatment decisions.
However, this data is not always easy to get. Dr. Daisy Dulay, Randall Town, Laura Shaw and Rosie Holmes set out to improve how the AED data is shared ....Read full story here > (originally published on Island Health's Medical Staff website.)

Medical staff collaborate on business plan to replace Cowichan District Hospital
Read More Read Less
Planning a hospital is a massive, complex undertaking involving collaboration by a multitude of stakeholders. Physicians have an important role to play to contribute clinical expertise to the planning as it occurs and before decisions are made, to ensure future services meet the needs of patients.
It’s why the Cowichan District Medical Society (CDMS) took the opportunity to engage physicians soon after the concept plan for a new hospital was approved by the province.
“The CDMS approached Island Health with an offer to support physician involvement in the development of the business plan,” notes Dr. David Robertson, Executive Medical Director for the region. “This offer was welcomed and has helped ensure robust input from the physicians during this early phase of the project.”
With Facility Engagement funding and engagement opportunities made possible through CDMS, physician/medical staff members are working together with administrators and nursing staff to help Island Health create the business plan for the new hospital. The plan will also include input from patients, local First Nation communities and community stakeholders.
Physicians/medical staff have opportunities to:
- be involved in discussions and attend meetings to provide input into the plan
- visit and learn from other hospitals to contribute ideas and learning
- research best practices in care delivery to contribute to design and functionality
The business plan is the 2nd of 5 phases for CDH redevelopment. Island Health will submit it to government for approval in fall of 2019.
See: CDH Redevelopment Phases, News and Cowichan Valley Health and Care Plan>

Comox/Campbell River: Facility Engagement Changed Everything
Read More Read Less~~When the Campbell River and Comox Valley Hospitals (one-hospital, two campuses) opened last October, the transition from the old St. Josephs’ Hospital was welcome, but rocky. The design of the new spaces were not as workable as expected, and patient flow and congestion challenges in the ER escalated within the first few weeks. Around the same time, patient visits increased significantly. “Within the first few weeks, the entire back half of the emergency room was filled up with admitted patients,” says Dr Albert Houlgrave, Emergency Room Physician and lead on this Quality Improvement project.
He explains that physicians and frontline staff were feeling stressed about the congestion and patient safety, but did not feel their concerns were being heard by health authority administrators who were not in the hospital every day. So they met on their own time to brainstorm solutions - a process that created good ideas, but also created some friction with the health authority counterparts, who were not involved in the discussions.
That’s when Facility Engagement came along, and the Physician Engagement Society of Courtney & Comox Initiative (PESCCI) was formed. The groups began to talk. Facility Engagement created a platform for dialogue between physicians and administrators to look at their common goals. “Facility Engagement funding relieved some of that pressure to be regularly volunteering our time and energy when so many of us were already extremely busy”, he says “And it created a culture where we could meet to discuss solutions to the problem and subsequently meet with administration to put those ideas into action.”
Once meetings started, improvements happened quickly: a dedicated trauma bay, a hot stroke protocol, simulation training, redeployed nursing support for waiting patients, improved hospital signage, a new paging system and space redesign for new beds. “It was great to have administration on our side to help free up space and make new space for beds.”
Physicians, nurses and unit clerks also began to review patient cases to find further improvements to flow and efficiency, and with administration, were able to put their ideas into action.
“While we have been working hard within the ER to improve the frontline work, we have also been reaching out to other departments.” said Dr Jennifer Laurence, the co-lead physician on this project, adding, “To date we have had the Laboratory Department, Maternal/Child, ICU, and the Medical/Surgical Unit invited to our quality meetings to review issues of concern regarding patient care and ongoing relationship building between our departments.”
Today, the situation has turned around completely. Communication and teamwork between physicians and administrators has grown, and the culture has evolved. “We have more time to give, and have been supported by PESSCI under the umbrella of quality improvement, flow and efficiency,” says, Dr. Houlgrave. “From there, it has blossomed into a multitude of mini-projects and ideas.”
Dustin Spratt , Manager Emergency & Critical Care, ICU for Campbell River and Comox Valley Hospitals notes that administrators and physicians are enjoying a good working relationship, close communication and regular meetings, and are now looking at collaborating across the two sites. “The importance of Facility Engagement is critical in providing good quality patient care,” he says. “We have front line clinical and administrative operational levels of responsibilities. And to make it function well, we need to have good communication and relationships. Through collaboration we’ve been very successful with managing the change, and have been able to put a lot of quality improvement into play. Everyone is now collaborating around quality goals and successfully managing important changes.”

Victoria physicians collaborate to improve endoscopy services
Read More Read LessAs part of the Facility Engagement Initiative at the Victoria General Hospital, a group of gastroenterologists identified a priority to schedule endoscopic (ERCP) procedures in a more efficient and effective way. In the past, there would have been significant roadblocks to this kind of change as it would involve adjusting staffing practices, hospital room allocation and more.
The project’s physician lead, Dr. Denis Petrunia, reported that the funding facilitated getting all of the physicians impacted by previous ERCP booking model to attend initial discussion and planning meetings. As a result of this, members of the administration became aware of the complex issues and were then motivated to support the changes recommended. The groups organized a series of meetings to discuss how to reorganize the ERCP scheduling.
As a result, changes in scheduling practices for weekday procedures have now been successfully implemented, and the group is in the process of evaluating the outcomes and cost savings over the next few months.

Bringing real meaning to the word ‘team’ in Victoria
Read More Read LessAt the Royal Jubilee/ Victoria General Hospitals, the Facility Engagement work brought together physicians and staff from the hospital and health authority who might not otherwise have been in the same room together. The physician lead, Dr. Bruce Wong, an emergency room doctor, was looking to access data to generate and test an algorithm to predict individual patients’ wait times when they present in the ER. A meeting was set up between the ER doctor and staff from Decision Support at Island Health.
Given an opportunity to meet, they discussed not only the data about ER wait times, but also the overall work done by Decision Support to inform the provision of health services. Dr. Wong also happened to be responsible for drawing up the schedule for all ER physicians, and commented that a heat map generated by Decision Support - showing times of day when patients most likely to leave the ER without being seen by a physician - had directly informed his scheduling practices.
The staff from Decision Support were delighted to hear that their reports had made an impact on health decisions; one data analyst said “We just crunch the numbers and write the reports, but it’s so exciting to hear from people who read them!” It was a mutually satisfying meeting for all present. The ER doctor left the meeting knowing more about the kind of data he could access and what the Decision Support staff could do to help, and the staff at Decision Support left with validation for what they’ve been doing and a greater understanding of the ER physicians’ needs.
- Northern Health
Working toward Cultural Safety and Cultural Humility in the ED
Read More Read LessPrince George Medical Staff Physician Association, University Hospital of Northern BC
 In 2021, the EQUIP Health Care research project conducted in three BC emergency departments including in Prince George, shared findings on health inequity issues that affect Indigenous people and others seeking care. It shone a light on opportunities for change in emergency departments, often the first point of entry for many people accessing medical care and inpatient treatments, and when patients are at their most vulnerable.
In 2021, the EQUIP Health Care research project conducted in three BC emergency departments including in Prince George, shared findings on health inequity issues that affect Indigenous people and others seeking care. It shone a light on opportunities for change in emergency departments, often the first point of entry for many people accessing medical care and inpatient treatments, and when patients are at their most vulnerable.The University Hospital of Northern BC (UHNBC) in Prince George is in a unique position to help create long-term and sustainable approaches to address these issues. It is the largest teaching hospital in Northern BC for health care providers of the future, and is located in the region with the highest Indigenous population in the province.
At the same time, the work of the Prince George Medical Staff Physician Association (PGMSPA) is a collaborative and integral part of helping to build toward equitable and culturally safe care.
Catalyst for change
A foundation for change was established in 2018 when Dr Terri Aldred[1] pioneered the PGMSPA’s Cultural Safety and Humility work (currently led by Dr Todd Alec). In 2019, ER physician Dr Christina Boucher began to lead the cultural safety and humility work in the Emergency Department (ED). Dr Boucher is a non-Indigenous person who seeks to be an ally and advocate for issues of inequity in health care delivery concerning Indigenous people.
With PGMSPA Facility Engagement funding to cover physician time, she took several steps to get started. She first spoke with Dr Aldred about her vision. “Dr Aldred told me about her group, the identified need for physician peer support in the ED. This foundational work helped guide me in developing my ED work.”
Dr Boucher reviewed the EQUIP research project to better understand specific health equity issues in the ED. She also gained insights from In Plain Sight "Addressing Indigenous-specific Racism and Discrimination in B.C. Health Care" that reported on issues of inequitable health care access and outcomes endured by Indigenous peoples in BC in health care settings.
Dr Boucher then connected to work being done in Northern Health to incorporate into planning, including initiatives and resources offered by Northern Health’s Indigenous Health team to support learning and self-reflective practice among all physicians and employees.
Building an inclusive working group with Indigenous voices
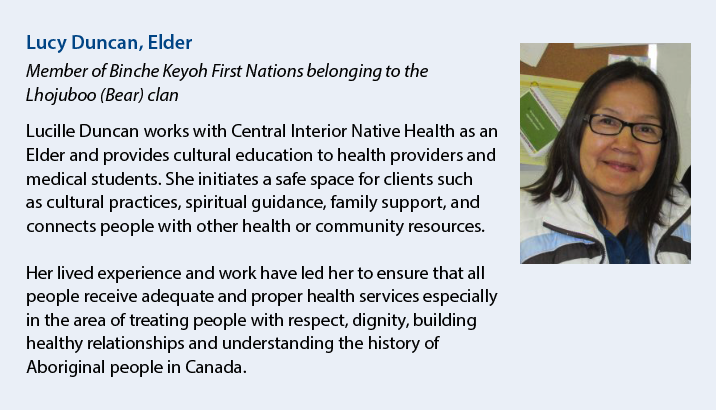
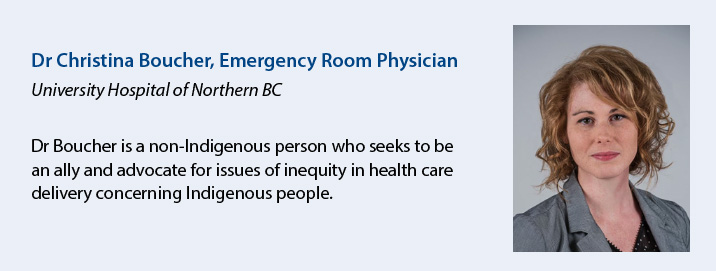 In order to foster and sustain change, full representation of all vested voices was needed to source and articulate issues and work together on solutions.Dr Boucher assembled a collaborative, diverse working group (see below) representative of virtually all interdisciplinary positions working in the ED.
In order to foster and sustain change, full representation of all vested voices was needed to source and articulate issues and work together on solutions.Dr Boucher assembled a collaborative, diverse working group (see below) representative of virtually all interdisciplinary positions working in the ED. Most importantly, the group needed to include Indigenous community members who rely on the ED and have lived experience as Indigenous people, whose participation required having trusted voices from the Indigenous community engaged in the work.
Through Dr Montana Halliday, Dr Boucher reached out to Lucy Duncan, an Elder working at the Central Interior Native Health Society and a well-known member of the Indigenous Prince George community. Lucy has also contributed to the EQUIP Health Care work, which seeks to ensure health equity within BC’s health care system.
Lucy joined the working group as an Elder and also spread the word to Indigenous community members to add their voices, particularly patients who experienced care in the hospital ED.
WORKING GROUP
- Elder, Central Interior Native Health Society
- 2 MSA physicians
- Northern Health staff: ED Program Leads (x2), Social Worker, ED Nurse, Acting ED Manager
- Indigenous Psychiatry Resident
- Indigenous patient
- Indigenous artist
- College of New Caledonia Aboriginal Resource Centre representative
- Former Chief, Stellat’en
- Elder Teacher, Lheidli T’enneh
- Aboriginal Patient Liaison
- Central Interior Native Health Services, Nurse Health Care Coordinator
- University of Northern BC / EQUIP researcher / Nurse Practitioner
"I was excited to join and expand on the work I’ve been doing with other health providers. It’s important to understand historical racism and its impact, if we want to build a better health care system that serves everyone.
...It is important to have Elders from the community with lived experiences as part of the group," she notes. "It is through their participation that open communication can happen about what Indigenous people want to experience in the ED and what barriers they have faced.” - Lucy Duncan
Feeling and finding purpose through truth telling and relationship building
The group agreed to meet monthly, and to start their work by creating an authentic foundation for change through relationship building and storytelling. The meetings place an emphasis on connection before content. Meetings start with introductions and check-ins, followed by open space for Elders and Indigenous community members to talk and share.
She emphasizes the importance of truth-telling to build understanding and support for action to address Indigenous-specific inequities in care. “The challenge is to be sure you are working on the real issues that will make culturally significant change – so it’s important to verify with the community."
"I have learned this year from the Elders on our group that relationships and trust are foundational, and are the most important activity when coming together as a group." - Dr Christina Boucher
Between meetings, Dr Boucher spends a lot of time checking in with each working group member about thoughts and feelings that have come up in the meetings. She notes that each person reacts differently, as personal, emotional stories are shared.
In her experience, she finds that talking about cultural safety and cultural humility can be challenging on a social and emotional level. It is a personal journey that takes time, and trust, and cannot be rushed."
It takes time to work through emotional contexts in order to even feel safe with one another, let alone to talk about all the details and processes involved in making the environment safe for all.
From there, the group can start to formulate action items that have arisen from the discussions.
"I see the activities of the working group prompting people in our department to engage in the self-reflective process of developing cultural humility.
Space and time are needed to build trust, create understanding, and shift beliefs to create sustainable change.“ - Dr Christina Boucher
Changing mindsets leading to positive change
The First Nations Health Authority's "Creating a Climate for Change" describes cultural humility as "a process of self-reflection to understand personal and systemic biases and to develop and maintain respectful processes and relationships based on mutual trust. Cultural humility involves humbly acknowledging oneself as a learner when it comes to understanding another’s experience."
Dr Boucher uses this sentiment to approach thinking about practical steps to take as a health care provider: “As a non-Indigenous person, I try to approach the world with an open curiosity. I hope to be an ally and advocate for the Indigenous people who are my patients, and my patients’ family members."
"I hope to continue working on identifying my personal biases and the systemic barriers that contribute to the inequity of care the Indigenous people have historically received, to make some positive improvements.”
Asked how this work could be expanded to other communities, Lucy Duncan says,“we need to build credibility with other communities by initiating the working group’s recommendations, such as an Indigenous Patient Liaison working in the ED, and showing the positive changes happening in Prince George.”
She hopes to one day see a health care system that puts aside personal biases, and provides care in a safe environment that includes dignity and respect.
"It is only through acknowledging our past can we move forward to a better future." - Lucy Duncan
Taking action: building blocks for change
Discussions have led to the following action items:
-
Plans to redesign the ED space to be more inviting to the Indigenous community, for example working with a local artist to create drums and relevant artwork.
-
Advocating with Northern Health for an ED-specific Indigenous Patient Liaison position who would assist indigenous patients to navigate through the ED and access care.
-
A proposal for cultural safety training for the security company working in the ED.
-
Using video monitors in the ED to display information about community resources and supports.
-
Sharing culturally significant learnings from the monthly meetings with ED doctors and nurses, as well as community urgent care clinics and physicians in other Northern Health hospitals and communities.
[1] Dr Terri-Leigh Aldred is the Medical Director for Primary Care for the First Nations Health Authority. She is leading community-based First Nations Primary Care Initiatives (FNPCI), as well as the First Nations Virtual Doctor of the Day (VDOD) and First Nations Virtual Substance Use and Psychiatry Services (VSUPS) to engage medical affairs matters related to our programs.
This work has been supported with funding from the Specialist Services Committee Facility Engagement Initiative, one of four joint initiatives of Doctors of BC and the Government of BC.

Prince Rupert: Creating space for better collaboration
Read More Read LessAs a small rural hospital, the Prince Rupert Regional Hospital relies heavily on a small, but mighty staff. Facility Engagement has played a role in helping their Operating Room (OR) staff build a greater and more collaborative environment. It started with a proposal for an OR improvement project, which was championed by Dr. Philip Nel, Dr. Meiring Joubert and Dr. Johannes Piek and submitted to Facility Engagement.
The proposal was to hold two Zoom meetings with all OR stakeholders including the GP anesthesiologists, the surgeons, the hospital booking staff, the OR nurses, the director of care, the hospital service administrator, and the medical office assistants to explore areas for improvement.
The first Zoom meeting occurred in mid-December and explored issues that have regularly come up around OR services. Having it facilitated by an independent facilitator allowed for robust discussions. As a result, a survey was developed with the facilitator and involving both the doctors and the Health Authority administration to determine what opinions needed to be captured.
The survey was administered to all Zoom meeting participants to help hone in on issues to be discussed and prioritized during the second Zoom meeting. The second meeting held in mid-January was fully attended by all previous participants.
Dr Piek noted, “we haven’t had everyone at the same table. Everyone was positive and enthusiastic, and everyone wanted to help and make things better. We now have a really positive and open communication forum.”
While many of the priority issues have to be put on the backburner during this time of COVID, there were positives that are helping to make small, but important improvements. A whatts app chat area has been established to allow for information sharing and to help set agendas for the Facility Engagement supported OR staff’s regular check-in meetings between the doctors and the health authority.
The meetings and the chat area have all contributed to a better understanding of everyone’s role. Dr Joubert observed, “for example, when a surgeon wants to do a small add-on to the OR slate, it is now with an understanding on how this apparent small change has an impact on readying pre-op patients for surgery, OR staff, in-hospital beds, and so on. We are all able to now understand each other’s roles and the impact of our actions.”
As COVID restrictions ease – there will be more opportunity for this close, collaborative OR group to address the bigger issues identified through their Facility Engagement activities. In the meantime, the open forum and regular meetings are a great launching pad to allow for a better understanding of the challenges and potential solutions.
Introduction of traditional foods to hospital connects happier patients with culture
Read More Read LessAt Northern Haida Gwaii Hospital in Masset, the introduction of locally-prepared and sourced traditional Haida foods to the hospital menu connected happy and grateful patients to their culture. In addition to increased patient satisfaction, the improvements in food quality also reduced costs by 20%.
In 2018, the Medical Staff Association and registered dietitian Tessie Harris embarked on a Facility Engagement project to restore on-site hospital food preparation, with a plan to integrate local and traditional foods.Haida Gwaii is home to the territory of the Haida Nation, where wild and traditional foods are abundant and an important part of the culture.
Prior to this project, the hospital had been serving retherm meals made elsewhere, delivered in individual portion sizes, and reheated for patients. There were patient complaints and low food satisfaction in surveys.
Serving up change
Although a small hospital serving 8 or 9 patients and residents, some big steps were needed to prepare meals on site.
To start, Tessie Harris liaised with Northern Health’s regional diet office in Prince George to align and coordinate the food service transition with Northern Health guidelines and processes. The site adopted the regional menu while incorporating traditional foods to reflect the needs and wishes of patients and respect local culture.
Staff then started cooking one meal a week on site, increasing the frequency over time. By the end of one year, they were cooking all of the patient meals in the Northern Haida Gwaii Hospital and Health Centre kitchen.
Traditional Haida foods were incorporated into the menu. Wild berries and greens were locally sourced. Arrangements were made with fishers in the area to catch salmon and halibut to be processed by local plants. They wanted support the hospital and patients, who were often their friends, family or neighbours.
Patients were happy and grateful. They commented about how much the food connected them to their families, culture and memories. They started eating more, and the amount of food returned to kitchen decreased.
Notably, while increasing the quality of the food – but without increasing staff levels – the site saw an approximately 20% reduction in food costs.
The success of the food service transition project has helped to influence a broader effort that continues in Haida Gwaii to integrate local and traditional foods into other areas of the community, and build capacity for a local, sustainable food system.
In our small rural hospital, improving quality of food served by resuming in-house cooking has had noticeably improved staff and patient morale. We are serving food that we want to eat!”
— Dr Caroline Walker, MSA President & Chief of Staff, Northern Haida Gwaii HospitalDietitians at the hospital continue to work with the community and Northern Health to increase the amount of local and traditional foods offered, an effort that reflects the greater focus within health care to provide patient-centered and culturally safe care.
"Patients light up when you serve food that reflects their culture. Nutrition is a big part of it, but the emotional, cultural and spiritual health and feeling of being connected is also making a difference.”
— Tessie Harris, Project Lead

Optimizing patient safety in multi-team obstetrical emergencies
Read More Read LessPhysicians at the University Hospital of Northern British Columbia in Prince George have been working with each other, administrators and frontline staff to improve team work and communication between the Departments of Obstetrics, Pediatrics and Emergency.
The goal: to work more efficiently with each other during emergency situations and provide better patient care, especially for high-risk obstetrical cases.
Communication errors can sometimes be a cause of perinatal death or injury during an obstetrical trauma. The departments involved wanted to reduce this risk by improving communication, fostering mutual respect, and by clarifying the designated roles of various member of the team.
Dr. Maria Odulio lead the way to bring together Obstetrics, Neonatal Intensive Care Unit, Emergency, Nursing and Respiratory Departments for a workshop. In total, 67 participants took part, representing:
- Physicians
- Midwives
- Nurses
- Respiratory technicians
- Unit Clerks
- Perinatal Council
- Risk Management
More than two-thirds of those who attended learned something new, such as helpful or critical information related to various codes (Code Pink , Code Blue, Code Neonate, etc.), the Respiratory role, the importance of a good patient handover, and the debriefing policy. They also learned the importance of clear, respectful communication and role clarity. In the future, more multidisciplinary simulations can be used to prepare for emergency situations.
‘I just wanted to say a big thanks for all the work you (Dr. Odulio) put into today. I thought it was a great success - a welcome start to important conversations and improved teamwork’ - ED Physician Participant
‘I just wanted to thank everyone again for a very successful workshop…the evaluations are overwhelmingly positive with 9-10/10 for helpfulness’ - Northern Health Clinical Nurse Educator

Onboarding supports give newly hired physicians more time to focus on patients
Read More Read LessA University Hospital of Northern British Columbia (UHNBC) and Prince George Medical Staff Physician Association (PGMSPA) collaboration
Working in different hospitals and locations comes as part of the training to be a physician, but once graduated things change. The supports and people who helped a physician to manage during training usually disappear.
UHNBC and PGMSPA recognized the need to have more supports in place to ensure new physician hires have as much time as possible to focus on patient care.
In 2021, they launched a joint onboarding project as part of a broader initiative undertaken by Northern Health for hiring medical staff. This is focused specifically on supporting newly hired physicians, many of whom have moved from other places in Canada, and even other countries – making them new to the community of Prince George as well as the hospital.
The project began with a job post for a single Physician Onboarding Champion to develop and implement a robust onboarding process to support physicians through their first year. Two physicians responded – family physician Dr. Lauren Feldhoff and general surgeon Dr. Erin Martin – and were hired to work together on the project, which brought several advantages.
They were both relatively new hires whose fresh knowledge of their experiences and combined perspectives as a GP and a Specialist helped create a more comprehensive and well-rounded onboarding process.

 “
“(Left to right Dr. Lauren Feldoff and Dr. Erin Martin)
Dr. Martin notes, “One of my experiences was being on call for Saturday and not getting my college licensing number until that Friday night – it was incredibly stressful and unnecessary.”
They began by investigating and analyzing the current supports available, which resulted in a 90-page comprehensive onboarding guide for physicians. Examples of items in this robust document include:
- links to many resources
- critical steps for licensing/credentialing, day-to-day practice tips
- information about how UHNBC specialities and services are organized to improve interprofessional team work, setting up charting and billing
- tips on how to open a practice (find space, hire staff, etc.)
- information about living in Prince George
It’s really a reality check about how much time this all takes. Brand new graduates don’t know how long it will take to get their license or how long it will take to get privileges or an MSP number.” - Dr Martin
Drs Feldhoff and Martin then conducted several focus groups with newly hired physicians, who were provided with a rough draft of the comprehensive onboarding guide to review before meeting.
“We talked about the goal of the document and explored where they found challenges with onboarding and what they would have liked to have seen done,” said Dr Feldhoff.
Drs Feldhoff and Martin noted that those in the focus groups said they wished they’d had the information when they first started because it would have made their lives much easier and allowed them to focus more on their patients rather than administrative issues.
Other concerns were raised during the focus groups that were outside the purview of the project, but impacted the work. Examples of these concerns included:
- access to clinic space
- access to child care
- scheduling surgical assists
- improved access to order sets and requisitions
- upgrading the UHNBC website
Drs Feldhoff and Martin documented these concerns for Northern Health, met with Department Heads for their feedback and made themselves available to work at addressing these additional issues. They recently received funding from PGMSPA to explore solutions to address the concerns, which includes piloting a surgical assist call schedule.
The final onboarding program is still in development. Plans include:
- holding an orientation week before physicians start their clinical obligations to spend time with IT and other relevant departments
- having some physicians dedicated to meeting new staff during orientation week to answer questions and get to know each other
- ensuring all administrative issues such as credentialling/licensing, parking passes, hospital swipe cards, etc. are in place
- holding regular check-ins with Drs Feldhoff and Martin during the first couple of months of starting work
Drs Feldhoff and Martin both agree that the best part of working on the project was getting to know each other. “It’s been great that the work we are doing is being appreciated and people are interested – so it’s very motivating to continue.”
They acknowledge the great support they received from PGMSPA through Renata Chapman, project manager and Dr Ian Schokking.
The work continues, and it is expected that newly hired physicians starting in 2022 will find their transition much smoother and their time better spent with patients and their care.
For a copy of the onboarding package, please contact engagement@doctorsofbc.ca.
The Prince George Medical Staff Physician Association is grateful for the funding provided by the Specialist Services Committee Facility Engagement Initiative to support these initiatives.

Same Day Shoulder Replacements: Reducing unnecessary hospitalizations
Read More Read LessDr Paul Van Zyl, an orthopedic surgeon in at the University Hospital of Northern BC (UHNBC) in Prince George had been reading all the literature about same day surgeries for total shoulder replacements. At Prince George, a total shoulder replacement, which is a complex procedure that involves replacing the shoulder joint with artificial parts, required overnight hospitalizations.
Dr Van Zyl along with four other Orthopedic Surgeons: Drs. Ashman, Dreyer, Mackey, and Purnell and two anesthetists: Drs. Dhadly and Phillips wanted to see change – and COVID-19 became the catalyst to initiate that change.
Dr Van Zyl notes, “The hospital was a COVID center, so scheduled elective, non-urgent surgeries were cancelled. As the pandemic continued, the waitlist for surgeries was growing.”
The timing was right to put same day surgery for shoulder replacements into action. “The problem with surgeons is we have good ideas, but we get busy and we run out of steam,” he says. “With a group like Facility Engagement, they keep everyone going. Facility Engagement staff, Project Manager Renata Chapman and Administrative Assistant Ardelle Bernardo helped me organize and get stuff done.”
With everyone focused on good ideas, they got it off the ground fairly quickly. In fact, they accomplished their goals after about four meetings. It started with identifying who needed to be involved including: surgeons, anesthesiologists, pain doctors, physiotherapist, OR nurses, peri-operative care nurses, and northern health administration. Dr Van Zyl notes, “Everyone really wanted to make this work – so it was an easy project.”
Jana O'Neill, Manager of Perioperative Services and Lia Clemas, UHNBC Director of Perioperative and High Intervention – along with their teams – were key partners in the success of the project. “We were fortunate that with a large multi-disciplinary team involved, we were still able to work quickly to accomplish the goal,” says Lia.
Shifting from traditional surgery to same day required changes in pre- and post-op care, as well as anesthesiology medicines. The big thing was post-op pain control and infections. To help the patient manage pain control, physiotherapists conduct a session with the patient and family before going home. A nurse follows up the next day by phone. Antibiotics are administered for infection control and there is a specific dressing that can be left on for a week to decrease exposure.
The group are currently tracking the data for pain control, infections and readmissions and there have been no red flags. Dr Van Zyl says, “We have done 14 surgeries since we started in November and no problems so far. I don’t foresee it being a problem – it hasn’t been with all the other studies.”
A spinoff from this project are day surgeries for hip and knee replacements with patients in an appropriate medical state. Dr Van Zyl has done some hip replacements already with great results. One of his patients who had both hips replaced - one following the traditional protocol with an overnight stay and the other as a day surgery, said she much preferred the day surgery.
Collaboration and engagement was a key success factor. “For me personally, Facility Engagement has really opened up the lines of communication between physicians and administration. It has brought a level of comfort to our working together" - Lia Clemas
In gathering feedback from all participants and stakeholders – it is clear that nothing succeeds like success – the general consensus is all are looking forward to collaborating on future initiatives and projects.

Lens replacement protocol helps the whole community
Read More Read LessLike many communities in BC, Terrace faces a shortage of family doctors and the local health care community is continually looking for ways to maximize capacity in primary care.
At Mills Memorial Hospital, physicians identified a way support these efforts, by streamlining the process for cataract surgeries which in turn, would reduce the number of visits patients need to make to their family doctor’s office before surgery.
Lens replacement surgery for cataracts is performed at the hospital about 97 days per year, with an average of 13 procedures performed each day. This adds up to roughly 1261 procedures per year performed in the hospital. And because patients need to be assessed by their family doctor before their surgery, the primary care appointments also add up, placing further pressure on wait times and access for other patients to a community GP.
Physicians at Mills Memorial Hospital identified that many of the patients’ pre-operative primary care visits for uncomplicated lens replacement procedure are unnecessary, or redundant. So the ophthalmology group and the surgical committee - led by Dr. Abe Torchinsky and Dr. Andrea Geller - along with the corporate executive lead for surgery and allied health staff, set out to streamline a pre-operative pathway.
They established a process that eliminates the need for a history and physical exam to be performed by the community GP. Instead, the Canadian Ophthalmological Society guideline which requires assessment of the patient by a health care provider can be met in the ophthalmologists’ office without the need to routinely involve GPs.
Encouraging and far-reaching results
The result? A limited trail involving a subset of patients attached to a family doctor in Terrace was successful in reducing the number of primary care visits needed for a pre-operative history and physical exam. A review of 4 slates of cataract surgery in May 2019 showed a total of 31 patients (65% of the total) were not sent to their GP prior to surgery.
With full adaptation of the changes in guidelines, it is estimated that more than 1200 primary health care appointments can be created in the region annually - appointments which would otherwise not be available.
The impact of this collaborative effort and its positive changes is far reaching. Freeing up appointment time in family practices will increase timely appointments and access for other patients, improve patient experiences, and increase productivity and cost efficiency in the system as a whole.
Next steps:
While this pilot project enjoyed the success of meeting its stated objectives, more quality improvement work is necessary to ensure sustainable and positive change. Areas of further research include an analysis of lens replacement slates over time, and an exploration of the patient experience. Additionally, ongoing dialogue and collaboration with Northern Health Administration and the Director of Care is necessary so that amendments to policies and procedures occur as a result of the project.

Physicians and Northern Health collaborate to introduce secure texting
Read More Read LessFor most of us, texting has become second nature as a fast and easy way to communicate. But in healthcare, technology has taken time to catch up.
“Physicians know that you can’t talk about sensitive confidential information through text messages,” said Dr Brian Hillhouse, and family doctor and emergency room physician at the University Hospital of Northern BC (UHNBC).
The advantages of texting however, he explained are many. Information is right in front of the doctor when needed. A text is less intrusive and more responsive than a phone call or voice mail, making it easier and faster to share information needed for patient care, especially when a timely response is needed. “It’s very efficient and handy for practice.”
Recognizing that texting could be an invaluable communication tool for doctors to use in their clinical work, Dr Hillhouse took the opportunity with Facility Engagement to initiate a collaborative project with Northern Health to create a secure texting app for physicians.
Getting on the same page
After doctors were polled to confirm that texting could improve their job functions, Dr Hillhouse, with six colleagues as fellow tech testers, and Northern Health’s IT department, embarked on a collaborative effort to see what could be done. The physician group discovered that Northern Health’s IT team had already been looking into technology options for secure texting. At the same time, the IT team did not realize that physicians were also interested.
“Things were so much better when we brought the IT developers and end users [doctors] together into the same room to look at the needs from our respective viewpoints,” he noted. “Physicians were able to explain their practical day-to-day needs, while IT was able to advise about functionality and appropriate use of the tool.”
Ron Klausing, a Project Manager for Northern Health IT, along with Dr. Bill Clifford, Northern Health’s Chief Medical Information Officer (CMIO), were a huge source of support. “As a former family doctor in town, Dr. Clifford understood where we were coming from,” he said.
The group first tested a application product ('app') already used by the hospital’s maternity and ICU departments and realized that it wasn’t a good fit. They settled on a product called MicroBloggingMD, which provided robust security features to meet BC’s privacy act. “We had a demo and a prototype period to try out the app,” said Hillhouse. “It worked better than we ever would have thought and had different functionalities that we didn’t even know we needed.”
Improving communication for patient care
As a start, doctors working in their community practices receive an alert when one of their patients is admitted to hospital. Then, as a big step forward, physicians working at the hospital can use the app to connect to the patient records system, so they can search for a patient’s name and be linked to the chart.
Physicians can also exchange information and photos securely with each other for consults and handovers, and communicate with nurses and residents. The app will soon notify doctors of critical lab results.
Dr Hillhouse said that radiology is one of the highest users. “We can alert them to prepare for an urgent CT, and get a text back about whether the scan is positive or negative.”
“So, it’s all in your pocket.” He noted that with pagers and voice mail, it isn’t always clear if communication has been received. “This way, we get acknowledgement when a message is read. So we know it has been dealt with and can worry about other things.”
The app also provides physicians with a way to get in touch with each other, bypassing the hospital switchboard. It includes a directory of all Northern Health departments and physicians, as well as an on-call schedule with clickable link, so physicians can connect with each other immediately.
Physician uptake
More than 50% of physicians have begun using the technology so far, with further adoption expected. “It is not our main and only way of communicating, but it is very convenient”, said Hillhouse. “It is an exciting opportunity to be able to use texting in medical practice in a secure and safe way, and one way of improving the efficiency of medical practice.”
He noted that the physician-health authority collaboration was a critical success factor. “Having end users working together with the design team will ultimately lead to higher uptake and satisfaction with the tool,” he said.
HOW IT WORKS
Information is transmitted through the app but is never stored within the app or in the company’s software, or on the phone itself, or in a cloud (such as Apple’s icloud).
All information flows through and is stored on Northern Health servers.
Security software is installed on phone itself and within the application, with a 6 digit passcode, facial recognition and encryption features.
Northern Health IT has ability to control the phone if lost or stolen including to lock or erase it.
All details of conversations are retained by Northern Health for legal purposes.
Application costs are based on inpatient beds, not the number of users, so everyone from physicians to nurses to students can use it without increasing costs.
Costs: Northern Health covered the app and project management, while physician time, coordination and engagement support staff costs were covered by Facility Engagement.
MSAs who wish to explore secure texting can get in contact with your Facility Engagement Liaison (FEL) for knowledge-sharing opportunities and to find out if your health authority or other sites have any plans in the works.
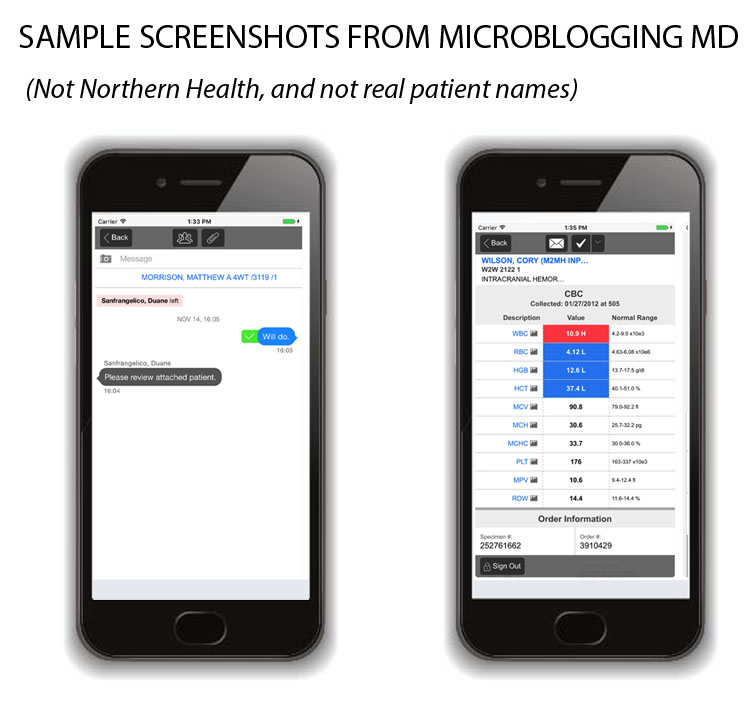

Facility Engagement improves teamwork & patient care in the North
Read More Read LessDr. John Smith, Past President of Medical Staff at the University Hospital of Northern British Columbia (UHNBC) and an internal medicine specialist has been a significant contributor to the work of Facility Engagement (FE) since its inception.
Dr. Smith says that Facility Engagement is allieviating some challenges at UNHBC. “Administrators are responsible for making budgetary and policy decisions, and the doctors are responsible for delivering [the expenditure [through patient care]. Yet none of the groups were talking to each other, which quite obviously was not leading to useful results.”
He says that as a solution, Facility Engagement has created opportunities and incentives for increased teamwork between the doctors and administrators, who no longer work in isolation. And benefits are showing in the areas of patient care, physician communication and relationships with staff and administration.
One example involves solving difficulties of getting adequate physician coverage for hospitalized patients, as GPs need to return to their individual family practices after morning hospital rounds and may be unable to return later in the day if needed. It is a common challenge at hospitals where GPs see inpatients. “If the physician is only at the hospital between 8:00 and 10:00 a.m., it’s very hard for teamwork, planning and multi-disciplinary rounds to occur.”
“As a solution, we consulted with physicians and Northern Health to establish a General Internal Medicine unit. It is a completely new structure developed to foster internal medical care, co-led by a doctor and an administrator.”
Under this unit, internists were recruited to look after the needs of hospitalized patients, and take pressures off of other GPs. The internist is able to make multiple rounds of patient visits, and address urgent concerns when needed in the middle of the day. With clear benefits for patient care, Northern Health was more than happy to collaborate on the project, and fund and sustain the new unit. “It’s simply a better system. The patients who are sick are looked after in a better way,” says Dr. Smith.
Another area of change he emphasized as a result of Facility Engagement has been improvements in physician communication. As an example, internists and family doctors felt that each did not understand the others’ pressures and needs. “With the help of Facility Engagement they came together, expressed their concerns and agreed on a set of rules. Recently [two years later] they have found they have greatly improved communication and collaboration.”
A third area where improved collaboration is growing is within the general hospital community that includes staff and administration. Last fall, the entire hospital community convened a “Change Day” in which physicians came together with staff pledged to change something in the hospital. “For the very first time something like this happened in Prince George and it was very successful,” he says. 296 pledges were collected, placing Prince George in fifth position in the province. The main outcome of the event was broad collaboration.
Now that internal collaboration is getting better established in UNHBC, plans are underway to broaden collaborative efforts through a planning session in which all hospitals in the region would take part. “At the moment, Prince George has a lot of effect on Fort St. John for example, but the latter has no real say in Prince George.”
Dr. Smith says that Facility Engagement is a “very sensible initiative. It has increased the number of physicians who are active in hospital improvements and activities. “If you told me three years ago that we’d have 40 per cent of physicians involved, I’d say ’no way’, but it is happening. The numbers fluctuate across different teams in the hospital.”
And even though he is soon retiring Dr. Smith says that with the exciting opportunities that Facility Engagement has created, “I would love to be starting again.”
Terrace physicians build teamwork with Northern Health partners
Read More Read LessSince January, there has been a big improvement in the relationship between the Terrace Physician Initiative Group Society (TPIGS) and their Northern Health partner, alongside other partners.
It all started when Dr. Lombard, TPIGS chair, began to meet with the Health Services Administrator, Chris Simms and Director of Care, Shirley Nichol in Northern Health on a monthly basis to discuss the development of FE work at Mills Memorial Hospital. This relationship, like any other, wasn’t without its road blocks. It took a collaborative effort from both sides to overcome pre-existing challenges.
Initially the two agreed that physician project proposals would be shared for feedback at the monthly meetings. This led to an open and mutual understanding between both the physician society and Northern Health about the projects and their implications on the site, staff and patients.
In the following months, TPIGS was faced with a challenge to implement two projects that required the participation of registered nurses. This was unanticipated and unplanned in the health authority’s annual budget – a learning that pointed out the need for closer collaboration.
As a way to initiate the needed collaboration, the TPIGS physicians, project manager, and Norther Health held a series of four meetings over the course of one week. In these meetings, Northern Health shared its strategic plan and improvement strategy to establish an understanding of priorities and possibilities, and align plans to prevent similar future challenges. TPIGS was also able to incorporate the health authority’s contributions into its own projects that were in planning stages.
The success of the team approach paved the way for a further collaborative process that was a first for both physicians and health authority. TPIGS physicians, Northern Health managers, and other partners came together at lunch meeting to discuss the integration of the physicians’ priorities with the health authority’s strategic plans for the north western region, which were displayed on the wall and reviewed by the group. Dr. Geller, TPIGS Treasurer, helped visualize how their physician-initiated projects fit into the health authority’s strategic plans. The physicians expressed their appreciation of the process and effort to respect and incorporate their priorities, and were amazed at how closely they resonated with TPIGS goals.
From its collaboration with Northern Health, TPIGS shares a few lessons that can be generalized for any healthy relationship: the earlier you start the collaboration the better, understand each other’s limitations and work around them; invest time in the planning phase to ensure future collaboration, meet regularly, whether formally or informally; align strategic plans; and seek opportunities for mutual gain.

Improving Quality of Care Across the North
Read More Read LessThe University Hospital of Northern British Columbia has been experiencing a year-by-year increase in acuity level of patients cared for by internal medicine services.
As a proactive measure to build and sustain capacity, and to ensure that medically-complex patients continue to receive high quality inpatient and outpatient care, members of the Department of Internal Medicine, Northern Health Authority and other physicians and stakeholders have embarked a three-point plan. It includes:
- Enhanced inpatient general internal medicine services, delivered by a multi-disciplinary team, to support patient admissions seven days a week.
- Coordinated outpatient care that includes clinics where there is little delay between when a patient is referred and seen for a consultation.
- Expanded weekday general internal medicine consultation services to support patients across the region using a broad range of distance services, such as video consults.
The plan, which will take about two years to implement, aims to improve the quality of care in both inpatient and outpatient settings. It will double the capacity of inpatient care, to sustain the availability of those services when needed. At the same time, it will establish a robust system of outpatient care to promote diagnoses of patients, and ensure they can get the care they need outside of the hospital, which in turn can reduce emergency room visits and hospitalizations.
The three components of the model provide a comprehensive solution to the unique challenges faced by the University Hospital of Northern British Columbia. A fulsome evaluation plan has been developed collaboratively by the physicians and health authority to measure progress and impact.
It is expected that the fruitful partnership of physicians working closely with health authority administrators to find solutions and develop a plan will be one of the key success factors of this initiative.
Internal Medicine Department physicians, University Hospital of Northern British Columbia. From left to right: Dr. Firas Mansour, Dr. John Smith and Dr. Anurag Singh. Absent: Drs. Amin Lakhani and Sharla Olson, Anne Chisholm (Health Services Administrator), Julie Dhaliwal (Manager Medicine)
- Providence Health Care

Taking engagement and leadership to the next level
Read More Read LessST. PAUL’S, MOUNT SAINT JOSEPH AND HOLY FAMILY HOSPITALS, VANCOUVER: Doctors working in Providence Health Care (PHC) have made big strides to strengthen their physician voice and community across the organization. Now, they are taking physician engagement to a new level.
The PHC Physicians & Surgeons Association and Medical Staff Association have been working hard to create interactive, meaningful opportunities for doctors to connect with each other, and to engage with senior executives and staff around mutual priorities.
Their efforts are paying off. The organization is listening.
As a key milestone, 120-plus physicians were engaged to contribute ideas to Providence Health Care’s new, seven-year strategic plan. It will pave the way to the opening of the new, state-of-the-art St. Paul’s Hospital in 2026 and the redevelopment of Mount Saint Joseph Hospital.
When the strategic plan was launched in mid-2019, a second phase of widespread medical staff engagement was initiated to apply its goals to physicians’ day-today work and patient care.
To support this process, six new Consultant Physician leaders funded through Facility Engagement, along with 25 physician advisors and health authority executive sponsors, have been leading medical staff engagement around each of the ‘strategic pillars’ and hospital redevelopment.
These roles are allowing for stronger representation, collaboration and communication among medical staff and clinical and corporate leaders as the strategic plan is put into action.
With this latest ground-breaking effort, Providence physicians and organizational leaders alike are excited about the possibilities that lie ahead, as they move forward together to build a world-class medical centre, research and academic health care organization.

Physicians meet to explore the future of digital health in BC
Read More Read Less"It doesn't matter what tools you are using, you can connect to peers and patients" - Dr. Douglas Kingsford
The digitization of health information is essential for us to have a sustainable health care system that can continue to provide British Columbians with quality care moving forward, says Dr. Douglas Kingsford, Chief Medical Information Officer for BC’s Provincial Digital Health Initiative.
Dr. Kingsford was a keynote panelist at the May 30 interactive 'Distinguished Speakers' dinner event hosted by the PHC Physicians and Surgeons Association (PASS) PIVOT Subcommittee. Providence physicians and CEO Fiona Dalton were joined by partners including Doctors of BC and Pathways to discuss BC’s plans for developing its digital health capabilities. It was one of many opportunities that Providence will have to collaborate and align the organization's needs, including its vision for the new St. Paul’s, with provincial and regional plans.
Dr. Kingsford, along with other panel guests, Dr. Damian Claydon-Platt - Chief Clinical Information Officer for VCH, PHC, and PHSA, and Brian Simmers - Chief Financial Officer for Providence, discussed the landscape in BC where, like in other provinces, digital health is fragmented. Health authorities, hospitals and community providers are often duplicating efforts and using systems and tools that aren’t linked together.
The Ministry of Health’s new strategy and governance for digital health across BC, along with the consolidation of regional IMIT services within PHSA, will change that. A coherent plan with short and long-term goals - and extensive collaboration among partners - will organize needs, streamline, modernize and link technologies together, and break down silos to ensure that everyone is working together to get more value for efforts. Ultimately, it will accelerate digital health capabilities in BC in a way that was not possible in the past.
A digital health ecosystem: an end to silos
Given the complexity of the health care system, there will not be a single digital health system for BC. Instead, a digital health ‘ecosystem’ will be created where data can move across the boundaries of multiple systems and vendors. “So it doesn't matter what tools you are using, you can connect to peers and patients,” says Dr. Kingsford.
Improving the exchange of clinical information will not only transform hospital-based care, it will support BC’s shift to increase comprehensive, team-based care in the community through Primary Care Networks. To be successful, physicians and multidisciplinary providers all need to be on the same page. Among other improvements, this shift aims to reduce preventable hospital visits.
Part of BC's digital health strategy also includes 'getting on top of' the explosion of direct-to-patient health empowerment tools, devices and apps in the marketplace - and determine how those fit into the medical landscape.
Importantly, there will be room for grassroots innovation to surface within the larger ecosystem. For example, if a group of physicians has an idea or need, there will be a way to propose, test and/or move it forward within the provincial/regional structure.
What's next?
Over time, as digital health evolves, physicians will start to see changes in areas such as patient information systems, secure texting communication, digital access to care, advanced QI data and analytics, medical technologies and artificial intelligence. All will transform care and how patients and providers experience the system.
Meanwhile, it is still early days. Health authority and technology partners, physician and patient groups, and others will collaborate around the path forward. As a start, physicians at the PHC May 30 event focused on providing feedback to Dr. Kingsford to help inform near-term actions. They explored physician ‘pain points’ and improvements needed, and answered questions about what priorities should be tackled first.
Moving forward, PASS PIVOT, as well as the Provincial Digital Health team, will continue to provide opportunities for physicians and leaders to engage in these discussions as they evolve and represent their needs and perspectives in the collaborative process along the way. Stay tuned.

Physicians weigh into health authority's seven year plan
Read More Read Less120+ Providence Health Care physicians engaged with the health authority to contribute priorities to the organization's 7-year strategic plan, which was released in spring 2019. Read more here >
- Provincial Health Services Authority

Building a Sustainable QI Network at BC Children’s Hospital
Read More Read LessThree pediatric physicians at the BC Children’s Hospital have a long-term vision to create a BC Pediatric Quality Improvement Practitioners (BCPQIP) Network. It brings physicians who have an interest in QI together on a regular basis to network with QI colleagues, share knowledge, receive guidance/advise and help further spread QI work.
Drs Tiffany Wong, Mia Remington and Sandesh Shivananda have all participated in QI in various ways, including through SSC’s Physician Quality Improvement (PQI) program.
Although there was a lot of QI work being done in the hospital – much of it was siloed. “We came together in a very organic way,” Dr Wong says. “Mia and I met through PQI and we met Sandesh through his work with the Hudson scholarship program, which is a program that allows junior physician scholars to focus on quality improvement one day a week over a two-year period.”
.
 .
. 

Left to right: Drs Tiffany Wong, Mia Remington and Sandesh Shivananda
Moving from silos to collaboration
Drs Wong, Remington and Shivananda acting as co-chairs began to build the network with funding from SSC’s Facility Engagement Initiative and Health System Redesign. They reached out to Quality Leads within each hospital division, physicians who have participated in PQI, Hudson scholars and others who expressed an interest in QI. Dr Remington notes, “We conducted a needs assessment survey before our first meeting because we didn’t believe the three of us should be setting the direction – it’s a shared experience.”
The survey responses helped to guide their first meeting in October 2020. There were about 27 physicians who all weighed ideas, expressed opinions and helped set priorities. Of course, all of this work was happening at the height of the pandemic, so Zoom meetings were core to furthering the development of the network.
Learnings from the survey and first meeting found that physicians wanted regular quarterly 90-minute meetings to share and receive feedback from QI colleagues on their projects, hear from QI experts and create partnerships for the spread of QI work across hospital programs. Physicians also wanted to foster engagement with the Health Authority (HA) Leaders and create a QI centre of excellence with ongoing operational funding. The co-chairs then prioritized their next steps.
The initial intention was to have the FE funding pay for speakers and some meetings held in a semi-formal atmosphere for face-to-face and network opportunities – but pandemic restrictions eliminated this approach. Two of the co-chairs went to the Institute for Healthcare Improvement (IHI) Annual conference in 2020 and identified some outside speakers, who they invited to present to the BCPQIP network. There have now been regular quarterly meetings held all through 2021 on Zoom with full attendance.
Dr Claire Seaton joined the network and says, “working in QI lends itself to collaboration, learning from others’ successes and failures, and getting feedback. The network gives us a space to do this, and has supported our efforts to be recognized for our work. I’m grateful to be a part of it.”
“We had a couple of HA Leaders invited to our meetings including Dr Felicia Lang, who is a Quality Lead within the health authority," Dr Remington notes. "She spoke to our group around quality structures – so it was a good opportunity to get to know each other.”
The next meeting is in April and for the first time it is planned to be a face-to-face dinner meeting with the goal of setting their direction for the coming year. Health Authority Lead Dr Derek Human is scheduled to share his experiences in QI, and also help members identify HA quality improvement initiatives that could be of interest to them.
“We don’t pay anyone to come to our events and they still come. I think they see value in being connected with like-minded colleagues,” he observes. “I think that is really powerful and valuable in itself.”
Success factors: connections, relationships, spread
The co-chairs agree that to be successful you need to really use your network, identify champions, and make meetings valuable so people want to attend.
Dr Shivananda notes, “We started this journey by nurturing connections and relationships between members. One of the challenges faced by our physician leaders is maintaining enthusiasm in driving change. Validation and appreciation of their efforts by peers helps everyone be resilient and remain engaged.”
Since the network has been established there have been a number of diverse QI projects presented and discussed, including a multi-disciplinary approach to asthma education, prescription medication equity and a parenteral nutrition program.
In addition, Dr Wong worked with the Faculty of Medicine DARPT committee to develop a promotions package where a doctor could be promoted based on QI work from Clinical Instructor right up to Full Professor.
“We developed a package with the DARPT committee and presented it to the pediatrics department,” she said. “They liked it so much they brought it to the Faculty of Medicine. After some revisions, it has been formally accepted. I’m very proud that health quality improvement, systems innovation and patient safety work is now formally recognized as important academic work.”
QI work will continue to be integral to delivering quality patient care and the BCPQIP Network is laying the groundwork for sustainable QI improvements in BC. Dr Shivananda is optimistic about the future. “We hope to strengthen the infrastructure for spread and scalability of innovative practices across the campus and beyond."
This work has been supported with funding from the Specialist Services Committee Facility Engagement Initiative and Health System Redesign. Both are joint initiatives of Doctors of BC and the Government of BC.
Pandemic validates engagement process for system improvements
Read More Read LessBCCDC Public Health Lab Client Engagement Feedback Project

In 2019, the BC Centre for Disease Control Public Health Laboratory (BCCDC PHL) set out to solicit stakeholder satisfaction feedback about current BCCDC PHL service delivery, with an eye to inform future service improvements.
As the province’s primary public health testing facility and microbiology reference lab for infectious diseases, the timing was fortuitous. COVID-19 would arrive on BC’s doorstep a few months later, shining a light on the laboratory’s essential role in enabling a coordinated provincial public health response to a global pandemic caused by an emerging pathogen.
Over the years, public health priorities and technologies had evolved, and the demand for PHL services had increased. Future modeling was needed to optimize services, turnaround times, operational and scientific capacity and resources, to effectively meet
the ongoing needs of the public, physicians and organizations across BC.
A pandemic was always on the radar as one of the laboratory’s many areas of focus. “Preparedness for a pandemic is one of the key priorities of a public health lab,” noted Dr Linda Hoang, Medical Microbiologist and Associate Medical Director and Program Head. “We were concerned about surge capacity and we wanted to find more efficient ways to streamline services.”
The PHL would need to tap into a wide variety of insights from BC physicians and organizations served by the laboratory to fully understand all of its strengths and opportunities for improvement.
So Dr Hoang – along with project co-leads, Dr Mel Krajden, Medical Director, BCCDC Public Health Laboratory and Karen Mooder, Director, Laboratory Operations – set in motion a BC-wide consultative process to identify PHL service expectations, gaps and challenges, and to seek potential solutions and recommendations from the clients themselves.
Engagement of this scale across a massive community of practice was no small undertaking, and Facility Engagement funding was key to enabling nimble deployment of resources to support realization of project outcomes.
The first step was to secure leadership for the project from Dr Perry Kendall, Clinical Professor at the School of Population and Public Health, and BC’s former Provincial Health Officer. Respected by administrators and physicians, Dr. Kendall is well-versed on the wide range of topics of interest across the public health landscape.
To support Dr. Kendall in facilitating dialogue across a diverse stakeholder group served by BCCDC PHL, a consultative framework was designed. Both clinically and operationally driven, it entailed dozens of one-on-one interviews and planning meetings that spanned five geographic health authorities, the Provincial Health Services Authority, and First Nations Health Authority (FNHA) and included:
- Public Health Managers
- Medical and Clinical Microbiology Team members
- BC Medical Health Officers
- 22 Physician participants including:
- General Practitioners
- Medical Microbiologists
- Infectious Disease physicians
- Physician Epidemiologists
- FNHA physicians
These consultation sessions also included senior operational and medical leads to provide appropriate clinical and operational context. All partners worked hand in hand with each other every step of the way, from project planning, to interview design, to communications.
“It was a true engagement effort, top to bottom,” said Jennifer Diep, Project Manager for BCCDC Facility Engagement. “Administrators and physicians always had an opportunity to provide feedback on an equal basis. It was very empowering.”
“It was everyone’s project – an operations project as much as a physicians’ project. That really improved connections, trust, and collaboration.” - Jennifer Diep
Further, when Dr Perry Kendall presented findings in a report, additional stakeholders were engaged, including scientists, public health students, laboratory trainees and administrators.

What did those findings show? Overall, a high level of satisfaction with the PHL service, including reference lab functions, expertise in interpretation of results, outbreak management support, and development of appropriate diagnostics. Concerns were also heard about the limited level of investment and lack of surge capacity at the time, and the need for a provincial strategy for diagnostic services and investments in future diagnostic and surveillance technologies, including genomics.
Many solid, specific recommendations were put forward for a future plan. But then, COVID-19 came along.
While there was no time to act on the report’s findings, the value of the engagement process was fully validated, as both the strengths and limitations heard from stakeholders were tested during the outbreak.
“The findings really showed up in this pandemic,” said Dr Hoang. “While we did not have the capacity and resources initially to get up to speed as quickly as we would have liked, our requests for resources were quickly supported, which allowed us to ramp up successfully. We had to re-organise our operational workflow very quickly, but we knew what was needed and thankfully, we were supported to do our job."
When the pandemic settles down, it is expected that PHL’s future planning will proceed, informed by the engagement process, as well as some new, real-life insights.
Dr Hoang noted that the COVID experience highlights some of the concerns about the limitations of the health care system that have been raised by those on the front line, further emphasizing the importance of continued collaboration between physicians and health authorities in health care planning.
“The system needs to trust in our expertise. By expanding these kinds of engagement opportunities, physicians will have an organized way to alert the health care system of deficiencies and red flags to improve patient and population care.” - Dr Linda Hoang

- Core Laboratory Functions
- Diagnostic services
- Communicable disease surveillance, prevention and control
- Outbreak and emergency response to communicable diseases
- Environmental health, drinking water and food safety
- Reference microbiology testing, specialized screening/surveillance, and diagnostic testing
- Biosafety, bio‐hazard containment and response
- Integrated communicable disease data management
- Public health policy development and evaluation
- Laboratory improvement and regulation (quality assurance)
- Training and education of healthcare and public health workers
- Public health related innovation, applied public health research and development

BC Children’s and Women’s Hospital highlights 30 FE projects
Read More Read LessThis summer, the Medical Allied Staff Engagement Society (MASES) of BC Children’s and Women’s Hospital held a Projects Day that highlighted the success 30 projects from the 2017-2019 round of Facility Engagement funding. Attendees, Hospital Administration, and fellow Investigators a glimpse into the great work being done by the MASES projects. Presentations, photos and project booklet here >
- Vancouver Coastal Health

Working to advance Indigenous cultural safety at Vancouver Acute and Community sites
Read More Read LessVANCOUVER ACUTE AND COMMUNITY: It’s well known that our province’s Indigenous peoples have worse health outcomes than our non-Indigenous citizens. The systemic racism that exists in our health-care system and in both acute and community settings has been part of the background to the UN Declaration on the Rights of Indigenous Peoples, the provincial bill to implement UNDRIP, and the In Plain Sight report.
 We need to increase cultural safety for Indigenous patients and family members in both acute and community care. How to do this is the mandate of the newly formed Vancouver Physician Staff Association (VPSA) Engaging Physicians in Indigenous Cultural Safety (EPIC) Task Group.
We need to increase cultural safety for Indigenous patients and family members in both acute and community care. How to do this is the mandate of the newly formed Vancouver Physician Staff Association (VPSA) Engaging Physicians in Indigenous Cultural Safety (EPIC) Task Group.Born from the iCON VCH Indigenous Health Rounds, the task group will prioritize and advance Indigenous cultural safety in health-care settings. It will be guided by meaningful partnerships with:
- VCH senior leadership and VCH Indigenous Health leadership
- VPSA physicians
- Indigenous Elders, Knowledge Keepers, physicians, patients, and communities
- First Nations Health Authority
- BC Ministry of Health
- UBC Digital Emergency Medicine Intercultural Online Health Network (iCON)
“The task group came about with collaboration between VCH Indigenous Health and iCON on Indigenous health rounds,” said Dr. Kendall Ho, an emergency physician and one of the task group founders. “VPSA helped fund these innovative meetings and we found over time growing interest from health-care professionals (physicians, nurses, and allied health staff). Close to 650 people registered for our last session, with 68 physicians attending. With that momentum, we worked with VPSA to establish the new task group.”
VPSA advocated for additional funding for the work the group will do. It has provided guidance and stewardship to ensure the task group’s goals align with the Facility Engagement Initiative’s mandate. VPSA also offers sessional funding for physicians attending task group meetings.
The outcomes from the iCON-VCH Indigenous Health Rounds have been impressive.
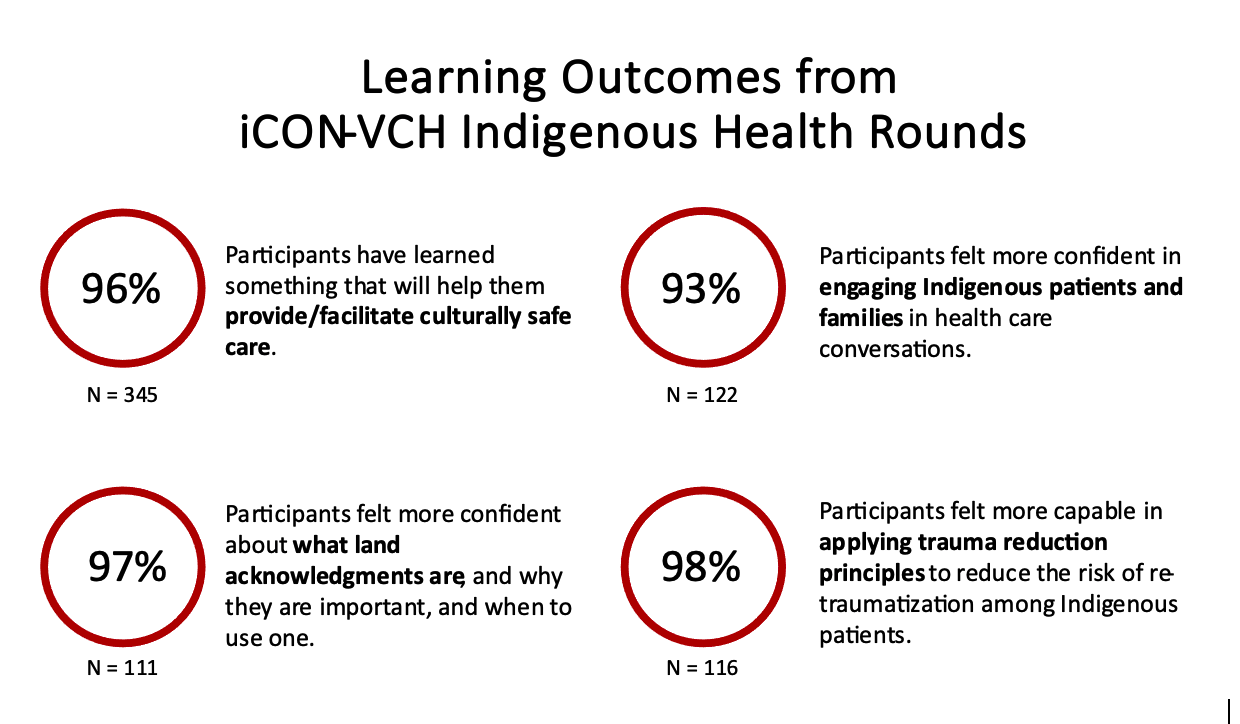
“Many of our physicians and health professional colleagues realize that even though we may not think we are racist, there is systemic racism and we, working in this system, sometimes display the behaviour of racism,” said Dr. Ho. “With that awareness, the majority of health-care professionals are interested in learning more to ensure all patients get optimal care.”
The EPIC Task Group has three key strategies for achieving its goals. These are continuing the iCON-VCH Indigenous health rounds, creating accredited educational resources, and developing a VCH Indigenous Health patient experience think tank.
VCH’s Vice President of Indigenous Health, Leslie Bonshor, is one of the executive sponsors of the EPIC Task Group. With her department, the task group is able to access and partner with Elders and Indigenous practitioners as well as engage with the First Nations Health Authority to make the health rounds good educational venues.
“Focusing on patients’ experience of care has to be a priority,” said Ms. Bonshor. “Physicians are used to questioning patients based on clinical experience, but we need to see a shift to understanding a patient’s experience of the health-care system as well in order to provide culturally safe care. This begins the moment an Indigenous patient walks through our doors.”
Ms. Bonshor and Dr. Ho are keen to share EPIC’s learnings with other health-care professionals across the province. Videos of previous Indigenous Health Rounds are available here, along with more information about them. Forthcoming educational resources will also be posted.
Dr. Ho’s hopes for the EPIC Task Group are high.
“I’d like to get to the point where Indigenous patients and caregivers feel free to come to us with no hesitation when they have health concerns, where they feel the health system is for them. It will be amazing when we get there.”
EPIC Task Group genesis
A chance encounter with an Indigenous patient visiting the VGH Emergency Department over 10 years ago set Dr. Kendall Ho on his “epic” journey.“The patient had been in a car accident, and I recommended X-rays for his neck,” recalled Dr. Ho. “He thanked me, but said he preferred traditional healing. It took me aback because I didn’t know what that meant. But it opened the opportunity for me to try to learn why he made that choice. It made me question my responsibility as a physician. I knew nothing about traditional healing, so as the hospital’s designated person in charge of this patient’s care, I felt incapable to decide if traditional healing was a suitable choice.”
Dr. Ho felt it was important to learn more. He was already working on the inter-Cultural On-line health Network (iCON) initiative and was in touch with Leslie Bonshor who was, at the time, the Indigenous senior leader in Fraser Health. He set off to help educate health-care professionals and himself to understand how we can approach and support our Indigenous patients better.
More than 10 years later, these initial steps led to the creation of VPSA’s EPIC Task Group.
Other ways VPSA is prioritizing cultural safety
Cultural safety for patients and health-care professionals is a top priority for VPSA. The association works closely with the VCH Medical Staff Diversity, Equity and Inclusion Steering Committee and several members sit on the committee and its three working groups. The committee’s purpose is to advance equity and inclusion for medical staff across the health authority and it achieves its mandate through a wide variety of activities.
Recent events that prioritize cultural safety include a presentation on creating a safe and inclusive space for transgender and two-spirit people by Dr. James Makokis and an Out Loud and Proud workshop during Pride Month on supporting 2SLGBTQIA+ people in clinical spaces.

Vancouver General Hospital Emergency Department takes on wellness
Read More Read LessDepartment-level strategies to address burnout
In 2019, VCH and the Vancouver Physician Staff Association (VPSA) joined forces to assess the level of burnout among physicians, to find its causes, and to develop collaborative solutions.
To understand what drives physician burnout and how that is different in every department, the resultant VA/VC Physician Wellness Steering Committee surveyed VPSA’s 1,900-plus members in October 2020. Since analyzing the results, the committee is meeting with department and division heads to determine next steps.
Applying the wellness strategy to the emergency department

The Vancouver General Hospital (VGH) Emergency Department was quick to act.
“Our group had the highest response rate to the survey,” said ED physician and steering committee co-chair Dr. Zafrina Poonja.
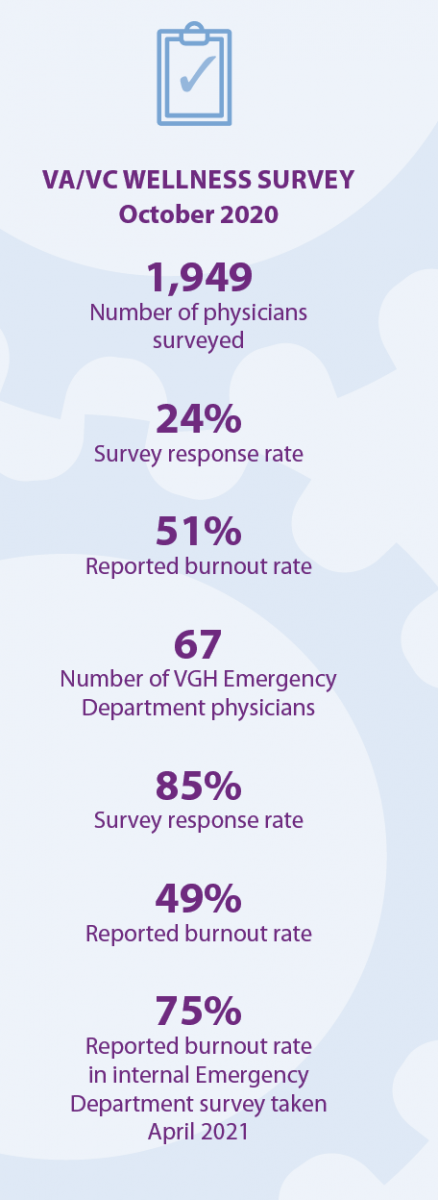 “We knew burnout was prevalent before the pandemic and that it was only going to get worse with COVID-19. Our burnout rate has skyrocketed over the past 18 months. The department realizes it needs to recover from its baseline rate plus the added stresses of the pandemic. We need to act now to ensure recovery.”
“We knew burnout was prevalent before the pandemic and that it was only going to get worse with COVID-19. Our burnout rate has skyrocketed over the past 18 months. The department realizes it needs to recover from its baseline rate plus the added stresses of the pandemic. We need to act now to ensure recovery.”How to do that and still function daily has been challenging. Four physicians volunteered as wellness champions: Dr. Poonja and Dr. Ka Wai Cheung; and department heads Dr. Heather Lindsay and Dr. Chris Lee.
They also take part on an interdisciplinary wellness team that includes nursing leadership. The group meets once a month. A departmental survey assessing physician wellness was conducted this past April and the nursing team will do its own departmental survey soon.
“Our role is to try to understand the best way to advocate for our own physicians in a challenging environment,” said Dr. Poonja.
“We need to shift the mindset to realize that when we look after ourselves better, we can better look after our patients. This needs to be done in a holistic way: as individuals; as a department; and advocating for the rest of the system. We need to identify and voice our concerns.”
Dr. Cheung agrees. “Every physician is in some way a wellness champion,” she said. “Every shift, my colleagues and I are identifying issues to look into and finding appropriate ways to address these. We’ve all experienced burnout and know there are things that can be done. Some are easier than others; we’ve also identified systemic areas that will require more work.”
Focused, manageable interventions relevant to department members
There are multiple quality improvement initiatives underway to improve ED physician wellness. These include improving the relationship between ED physicians and consultants, arranging more streamlined outpatient clinics, and changing how shifts are scheduled. Optimizing space within the department is another project the group feels it can address.
Dr. Cheung gives an example of one initiative that has resulted in her work becoming more effective.
“Sone radiology processes were not efficient from our perspective. We organized a meeting with the department and now things are running more smoothly.”
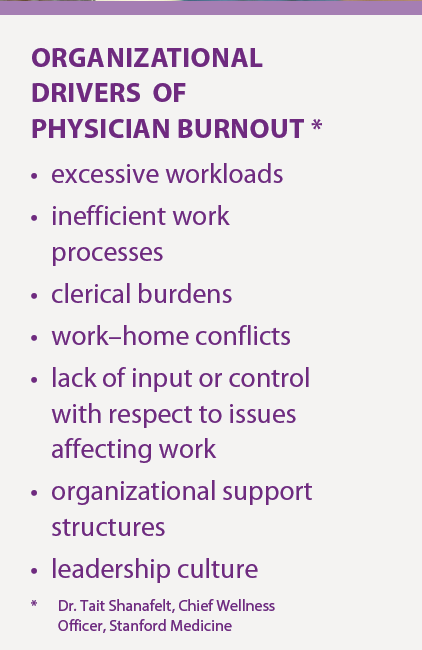 The department intends to apply for funding to address some of the deeper systemic issues that are drivers of burnout (e.g., workload) and is identifying champions to lead these.
The department intends to apply for funding to address some of the deeper systemic issues that are drivers of burnout (e.g., workload) and is identifying champions to lead these.“We use Dr. Tait Shanafelt and Dr. Stephen Swensen’s list of drivers of burnout to assess how we’re doing," adds Dr. Poonja.
“We’re doing well in terms of a sense of community within our group; we have a number of interventions in place for this," says Dr. Poonja. "Patient load and administrative work are higher burnout drivers for us. Our survey has provided us with specific examples of this and we’re looking to categorize these results to see what we can take on.”
This work is still in its early stages and Dr. Poonja acknowledges that while the micro interventions they have taken may have been helpful, the major stresses she and her colleagues face are overwhelming.
The work continues. Some further interventions may be within the control of the department, while others require change at organizational and system levels.
I tell myself how much worse things would be if we hadn't taken these steps - Dr. Poonja
“Burnout has been a systemic problem for healthcare providers for a long time, but the stresses of COVID have been an extra burden,” said Dr. Cheung.
“As frontline workers, we’re often the first to feel the burden but we don’t need to stay silent. There is a lot that can done. We can tackle this head on to the benefit of our colleagues and our patients.”
“Prioritizing physician safety and care would enhance everyone’s care,” emphasized Dr. Poonja. “Wellness is definitely a big priority for my department, and I’m encouraged that VCH seems to be stepping up.”
For more information and resources including Drs Shanafelt and Swenson's Mayo Clinic Strategies to Reduce Burnout>
This work is supported by Facility Engagement, an initiative of the Specialist Services Committee, one of four joint collaborative committees that represent a partnership of the Government of BC and Doctors of BC.

Physician-led lung cancer pathway reduces time to treatment for patients
Read More Read LessOver the past decade, options for the diagnosis and treatment of lung cancer have expanded rapidly. While that’s good news for patients, the health care system hasn’t always kept pace with the moving parts. Oncologists have been challenged to get the diagnostic information they need in a timely way to start treatment with patients. And with lung cancer, there’s no time to lose.
It’s why Dr. Jeremy Ho, an Oncologist at Richmond Hospital (RH) paired up with Dr. Karen Ung, an RH Pathologist, to engage interdisciplinary colleagues in the creation of a new pathway for the diagnosis and treatment of lung cancer. Together, they reduced the average turnaround time from biopsy to treatment from 55.7 days to 34.5 days – a drop of more than 21 days - a stellar success that has potential to be used for other cancers and at other hospitals.
Wait times for patients: not acceptable
Dr. Ho explains that a patient who presents to their family doctor or the emergency room needs to pass through a number of tests and specialists. They might get a CT scan, see a respirologist, get a bronchoscopy, an EBUS or a CT guided biopsy. But it doesn’t stop there.
“It’s not sufficient now to get just a biopsy that says ‘lung cancer’. Cancer care is very protocolized; we have to be strategic in how we plan our treatments. So we need to send tissue off to the BC Cancer Agency (BCCA) for more tests; to do biomarker or molecular testing and look at the specifics of the cancer itself. That tells us what treatments are best directed at it.”
The back and forth takes time, and Dr. Ho says the process was cumbersome. Ideally, oncologists should have all of the information needed for a treatment plan at the first appointment; but in reality, it could take up to eight weeks to get that information back.
“That is obviously a very long time when we’re dealing with an aggressive type of cancer. Families don’t understand why things are taking so long. Imagine you get a shocking diagnosis, and someone tells you, ‘we’re going to have to wait another one or two months for your molecular results to come back before we can plan for treatment’.”
“I can try to explain and address their anxieties, but at the end of the day, I agree, it’s too long,” he says. And just because it’s the way it’s always been, it doesn’t mean we just have to accept it.”
He discussed the problem with Dr. Karen Ung, who drew inspiration from developments in breast cancer diagnosis and treatment. “It used to be all over the place, but now has a standard of care. So how can we do the same for lung cancer? What can we do to make the process more streamlined to gain some time for our patients?”
Engaging colleagues and partners in solutionsWith the support of the Richmond Hospital Physician Society Facility Engagement funding and a project manager – they brought together cancer specialists from RH Radiology, Respirology, Oncology and Pathology to talk. Each typically provided services independently, but this was an opportunity to work together as a coordinated, comprehensive team to improve diagnoses and management pathway for patients. BCCA joined the discussions as a key diagnostic partner.
Over three multidisciplinary meetings held between November 2019 to February 2020, they laid out the pathway visually to consider barriers and solutions to save time and improve the standard of care: How long from when the patient first presents with either cough or a lung nodule to when they first get the first treatment? What are the steps? What is the speed of the tumor sample getting to the BCCA?
Discussions were eye-opening. Hearing from each other’s perspectives served to flag mistaken assumptions about what actually happens along the patient pathway, and increased everyone’s knowledge about respective roles and requests. Physicians started to see themselves in the bigger picture and the impact of each of their decisions on the overall patient journey.They identified where delays were occurring, and where small shifts in each of their roles could make a difference. Examples ranged from having respirologists take multiple biopsy tissue in the initial diagnostic for BCCA molecular testing; to having investigations occur in parallel instead of waiting for one test result before performing the next; to improving coordination of processes with the BCCA.
In 2020, the collective efficiencies started to add up. Dr. Ho says: “I was hearing less of, ‘Why are the results not here yet?’”
But even more telling was the data. It showed the turnaround time from biopsy to starting treatment had been reduced from 55.7 days to 34.5 days – a drop of more than 21 days. “We didn’t think that we would see something as dramatic as we did.”
The bigger picture
What’s next? Plans include looping in emergency department colleagues, and reaching out to the community family physicians to further refine the pathway. There’s also potential for scalability.
“This success gives us the momentum to be able to keep doing it for other things – apply to other oncological treatments that might use this similar type of testing,” says Dr. Ung. “It’s portable and replicable across everyone in the community or in a big centre.”
“While we made individual changes, we’re hoping for more systematic changes. It is good to shine light on the system itself, because ultimately, our patients benefit from it.”
WHAT FACTORS MADE THIS PROJECT A SUCCESS?
The passion and interest of physicians who want to do better: Dr. Ung: “A big highlight is that these efficiencies were gained, and in the end it doesn’t really matter if people are remunerated. Because we see that there’s an impact to the hospital, the work, and the patient, ultimately.”
A supportive provincial partner: Dr. Ung: “A BC Cancer Agency partner who was passionate and eager to align goals and priorities. In the past this was not possible.”
RHPS Facility Engagement Funding: Dr. Ung: “Funding was fuel and allowed for a venue to happen.”
A project coordinator who pushed for meetings, navigated the project pieces and data gathering (arranged separately from Facility Engagement). Dr. Ho: “Without that role, it is likely we all would have met, had one meeting, discussed the problems, and then it would likely have languished.”
Data collection: Dr. Ung: “It reinforces that we’re on the right track; keeps the momentum going.”

Finding common ground: Collaboration increasing between VPSA physicians and their health authority
Read More Read LessEvery month leaders from the 1,900-member Vancouver Physician Staff Authority (VPSA) and Vancouver Coastal Health (VCH) sit down to talk over mutual issues. They come to each meeting with an intentional focus that was agreed to by both groups and they rotate who chairs the meeting between VCH Interim President and CEO Vivian Eliopoulos and VPSA Managing Director Dr. York Hsiang. There is lots to talk about; both see physician wellness as a priority and they are also both invested in ensuring diversity, equity and inclusion among medical staff, and—for the past year—quickly communicating news regarding COVID-19.
VCH Physician Wellness Steering Committee
Since its start, VPSA has intentionally focused a large part of its work on wellness. In 2019, the health authority suggested combining forces to assess the level of burnout amongst physicians, to find its causes, and to develop collaborative solutions. The VCH Physician Wellness Steering Committee was formed with five health authority representatives and 12 VPSA members.
“We quickly realized we needed to understand what drives physician burnout and how that is different in every department,” said committee co-chair Dr. Zafrina Poonja. “We surveyed members in late 2020 and are now reviewing the data.”
Dr. Poonja credits the interdisciplinary composition of the committee with its ability to move the issues of physician wellness forward.
“We each bring a different perspective and it’s been important to have the support of VCH leadership. The health authority is invested in this issue and wants to do more so we can all be well; they’ve been very supportive. There are no quick fixes; there are issues within our system and within health care that are long standing. But if we can target micro interventions there could be a domino effect. It will take a lot of time and many grassroots initiatives, but my participation on this committee has made me hopeful.”

Communicating unexpected outcomes
Not all medical procedures go as intended and it is often left to physicians to deliver distressing news. It is therefore vital that physicians know how to communicate unanticipated results in a sensitive manner. VCH reached out to VPSA for help with this as it is a concern for both physicians and the health authority. VPSA funded a select group of skilled physicians to attend Communication of Unanticipated Outcomes in Healthcare training in fall 2020, thus developing an inhouse group of experts who will now teach the course to other physicians and health-care teams across the region.
“Partnering with VPSA on this project was paramount to ensuring physician engagement and collaboration,” said VCH Regional Director, Patient Experience Elizabeth Baron. “As we learn more about how to better include physicians as a part of our health-care teams and represent a cohesive approach to communicating with patients and families, we hope to see improved experiences for everyone. The impact of improved disclosure conversations—in addition to it being the right thing to do—has been shown to build trust in the organization, reduce fear of blame, decrease litigation against providers and the organization, and also shed light on organizational opportunities for improvement.”
“This project was a great example of recognizing a problem common to both physicians and the health authority, developing a response, and enacting solutions,” added Dr. Hsiang. “The educational leadership we’re creating will lead to improved communication skills that will ultimately benefit patients and their families.”
Later this year, the physician trainers will begin training their colleagues in communicating unanticipated medical outcomes.
Improving equity and inclusion in medical leadership
In January 2019, VPSA hosted an appreciative inquiry into meaningful leadership experiences and opportunities for women physicians. That work inspired the creation of the VCH Medical Staff Diversity, Equity and Inclusion (DEI) initiative. Eleven physician members sit on the committee along with four VCH medical leaders. The group’s work has earned praise from top VCH leadership including its board and interim president and it has changed the way VCH recruits medical leaders.
Over the past year, the committee held focus groups with women physicians about their experiences during the pandemic and it developed and launched a diversity survey to all VCH medical staff. It is about to begin physician Indigenous, Black and People of Colour focus groups and is planning an International Women’s Day event on gender equity in medicine.
“World events have made an impact on our work and there is broad interest in seeing DEI issues move forward at VCH,” commented committee member Dr. Joy Masuhara. “The health authority has started an organization-wide strategy and has valued getting physician input and feedback. We’ve taken a very co-creative approach and I feel that participating on the committee has helped foster better relationships between our groups. VCH is a large, complex organization and I have a better understanding now of the broader context for this work.”
“Without support from the VPSA committee members, the ability to influence a culture of change within the medical staff would be more challenging,” added VCH Manager of Physician Engagement Neli Remo. “The VPSA members have demonstrated courage and commitment to propel the DEI work to organization-wide levels and they continue to work tirelessly to advance and co-create an inclusive workplace.”
Welcoming new physicians to VCH
VPSA regularly hosts Meet and Greet events for onboarding physicians; its September 2020 event was held virtually via Zoom.
“Over 100 physicians joined our association in 2020 and we felt it was especially important to make them feel part of a community,” said Dr. Hsiang. “The pandemic has isolated us more than ever and we believe it is critical that we continue to take steps to break down silos between departments and divisions.”
VCH senior leaders attend these onboarding events and offer welcoming words. At the February 2019 event, Vivian Eliopoulos made these remarks:
“Our organization is our house and we need to have open and honest conversations about how we can make it the best possible place to be. There are discussions happening today that didn’t exist in a coordinated way before VPSA was formed and there’s a palpable energy encouraging us all to connect, collaborate and care. But [VCH leaders] can’t fix what we don’t know is broken. We want to hear from you so we can partner to make improvements.”
VPSA and VCH are now collaborating to survey newer staff to get a sense of what their pain points are in the onboarding process. The data will be used to craft solutions and improve their experience.
Communicating during a pandemic
There’s nothing like a common enemy to bring people closer together. A silver lining of COVID-19 has been the co-operation that it has brought about between groups like VCH and VPSA.
“We knew we would need to provide physicians with information about the virus that the hospital would be too busy to communicate,” said Dr. Vivian Yin. She and Dr. Sophia Park, who were both VPSA board members at the time, pulled information from the BCCDC and WHO websites and started a WhatsApp forum that touched on many COVID-19-related issues.
“VCH leaders were paying attention to WhatsApp and were impressed with how we were moderating it; they asked us to help them with physician communication. It was a timely request as we quickly outgrew WhatsApp and transitioned to the Slack platform that VCH medical staff continue to use to this day. VCH took over the platform and VPSA continues to provide support.”
The Slack channel has had a tremendous impact on physician engagement with specialists from various departments and divisions sharing knowledge rather than working in silos. Bridges have been built and leaders have emerged; it has also created a sense of community.
Early in the pandemic, VCH offered all-staff townhalls to update workers on the impact of COVID-19 on its sites. However, the information that physicians needed was different from that of, for example, nurses. VCH medical leaders Drs. Patty Daly and Chad Kim Sing understood that perspective and were amenable to suggestions for forums specifically targeted to medical staff. COVID-19 Virtual Medical Staff Forums debuted in March 2020 and have run regularly. Vancouver Acute also started offering a regular VA update.
Drs. Yin and Park were instrumental in the forums’ early days. They worked out the logistics and made sure physicians’ questions were gathered ahead of time.
“We stressed that all questions needed to be answered—even if it was only to acknowledge that they didn’t have an answer,” remembered Dr. Yin. “It’s increased the health authority’s transparency and it’s been new territory for VCH, which isn’t used to sharing so much information.”
“Medical staff communications have been well received during COVID-19 and these medical staff forums are a part of that,” said Dr. Kim Sing. “These efforts have led to deeper and more meaningful engagement and we’ve been able to continually improve our dialogue and communication with and between our medical staff colleagues.”
There is interest in continuing the medical staff forums in the post-pandemic world. The format and frequency may change but, in Dr. Yin’s eyes, COVID-19 has opened the VCH leadership’s mindset to getting more physician input.
Vivian Eliopoulos agrees. “One of the positive things around the pandemic is the networking across the organization that has occurred and it’s something we certainly want to continue,” she said. “My hope is that our forums don’t stop. Eventually we’ll move away from talking about COVID and vaccine planning into other areas of interest for our physicians.”

Vancouver MSA defines meaningful physician engagement
Read More Read LessVANCOUVER ACUTE AND VANCOUVER COMMUNITIES OF CARE: Members of the Vancouver Physician Staff Association (VPSA) developed a physician charter to enhance and guide interaction between the medical, dental and allied health staff and senior leadership.
The charter, which outlines a framework for physician engagement, was adopted by both organizations at a joint session in April 2019 and served as the basis for an article published by the Royal College of Physicians in July 2019.
“Widespread physician engagement across an organization leads to improved patient care, enhanced well being for physicians, and safer, more efficient, and less costly healthcare,” said Dr Simon Rabkin, VPSA’s immediate past president, and the article’s lead author.
VPSA’s executive and its advocacy committee created a draft charter that was circulated to its 1,900-plus members and presented at a Medical Staff Association quarterly meeting. Member feedback was incorporated into a final document that was submitted to VCH senior management.
VPSA’s engagement framework is based on one developed by the International Association for Public Participation (which other MSAs are also starting to adopt). It allows for several levels of engagement from inform (the lowest level) to consult, involve, collarborate, and empower. The closer an initiative comes to the empower level, the more influence stakeholders have. Higher levels of engagement require more time and resources and are rewarded by greater involvement and commitment of physicians.
LEVELS OF STAKEHOLDER INFLUENCE
• Inform: Stakeholders receive information and announcements
• Consult: Stakeholders are consulted on draft plans or on issues; feedback impacts decisions
• Involve: System involves stakeholders in planning and policy processes
• Collaborate: Stakeholders share decision making with their institutions
• Empower: Stakeholders identify issues, solutions, and actions with institutional support"The framework builds trust and offers a common language as well as structure, accountability, and transparency. Adopting it requires a change in organizational culture as well as a time commitment.”
— Dr Simon Rabkin, VPSA Past President
Meaningful engagement
To be effective, physician engagement must be meaningful. This includes broad and diverse involvement from the physician community as well as physicians’ ability to influence decisions and affect outcomes.
It needs to recognize and respect schedules. Physicians need to be given advance notice of new projects and policies to allow for optimal input. It should not be a single physician volunteering to work with administration or a single medical/surgical lead in the organization.Rather, the best outcome is attained when there is a balanced representation from all physician stakeholders who may be affected by the decision or change.
“Our goal is to support the greatest level of engagement possible and to build capacity, both within VCH and within our physician community,” said Dr Rabkin. “We want to partner with VCH leadership to achieve the best health outcomes for our patients.”The COVID-19 pandemic highlights the benefits to the health authority of engaging frontline workers to gain their feedback and assessments, which contributes to optimal patient care and to gaining the commitment of physicians to put their own health at risk during the crisis, according to Dr Rabkin.
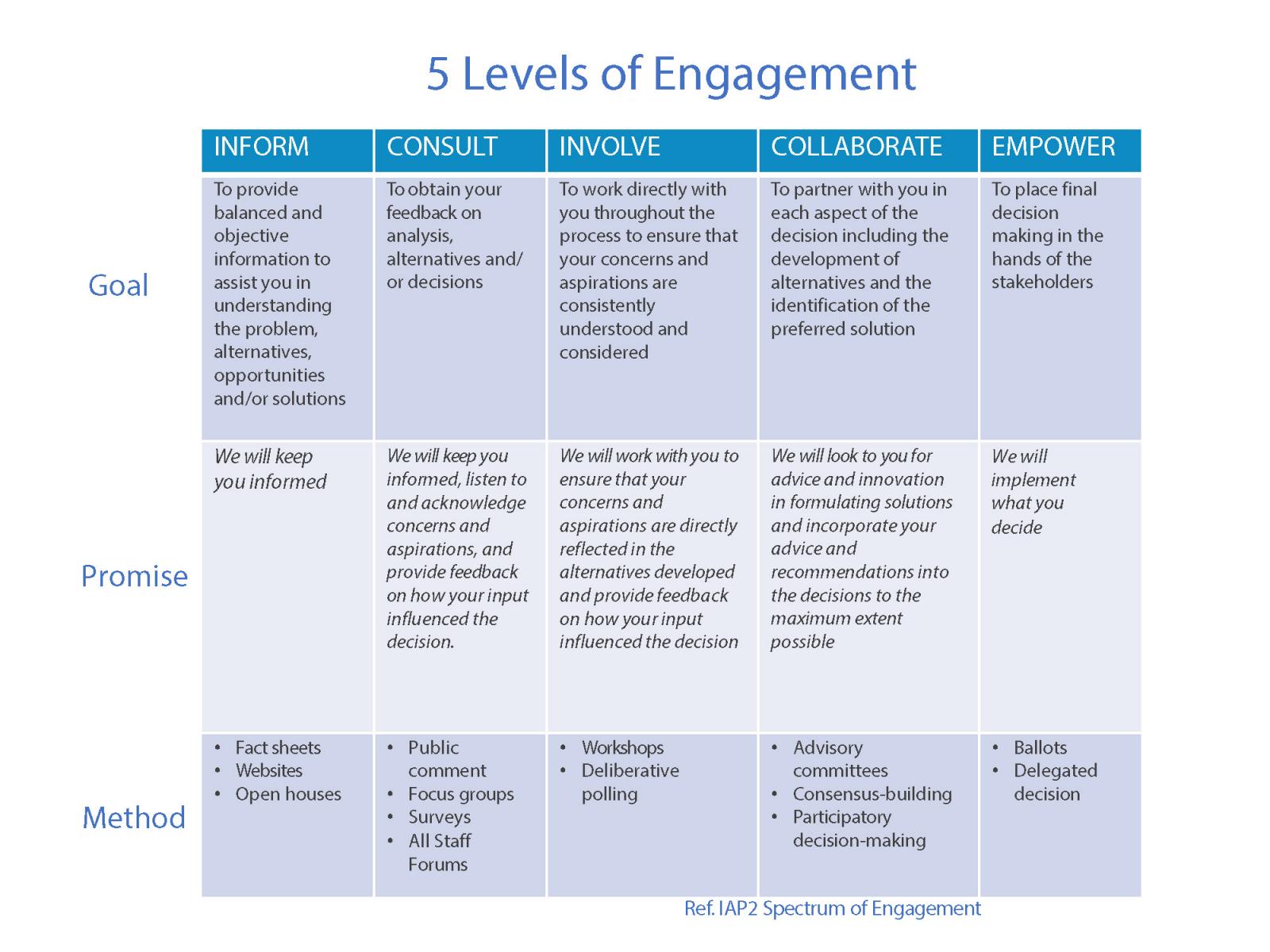
Next steps
Establishing the charter was an essential step towards meaningful engagement of VPSA’s physicians. It is top of mind for the association’s executive at their regular meetings with VCH’s senior leadership team.
VCH is committed to physician engagement and further dialogue is anticipated to implement processes and structures to embed meaningful physician engagement at all levels.
Read Journal Article here >
Team effort leads to $90K cost savings
Read More Read LessFrom a simple idea, great things can be accomplished. Just ask Dr Jin Ho. He saved almost $90,000 a year within the Endoscopy Unit at Lion’s Gate Hospital.
Dr Ho, Head Division of Gastroenterology at Lions Gate Hospital believed that there were significant potential savings within the Endoscopy Unit’s expenditure - he just needed the time and resources for a project to help him prove it and execute change.
As with many BC hospitals, budgets are tight and additional money for one-off projects are scarce. So, when Facility Engagement put out a call for project submissions that they would consider funding, Dr. Ho jumped at the opportunity. He put his proposal together, made his presentation to the Physician Engagement committee and received the requested funding for his project.
Dr Ho notes, “I always felt we could do our share in helping to manage our costs through competitive pricing of high volume, as well as high cost items we use regularly in our work.”
He gathered a small team of two nurses to price equipment and accessories used by the Unit. They then put out bids to vendors, negotiated prices, trialed new products, gathered feedback and implemented changes that resulted in savings without compromising quality and patient care.
Karen Cordner, RN and Patient Care Coordinator for the Unit who was on the team said, “The entire team was engaged in the process and became more conscious about costs. They were involved every step of the way on how the Unit could reduce unnecessary expenditures."
In addition, the team took on the responsibility of ordering some of the Unit’s supplies instead of it being the responsibility of the Medical Device Reprocessing (MDR) Unit. MDR supported this – recognizing the staff in the Endoscopy Unit have a better idea of the quantity of supplies needed. This change saw items ordered in a timelier fashion, and avoided over-orders and being left with expired, unused supplies.
The Unit is now saving almost $90,000 each year from the changes implemented and they have identified possible further savings of over $50,000 a year, by potentially switching to a new provider for endoscopic accessories.
Dr Ho’s next focus is to raise awareness of the costs of items used in the Unit with staff (physicians and nurses) by putting up posters in procedure rooms and around the Unit with itemized costs of the commonly used accessories. Dr Ho, “I hope this will help encourage members of staff to think twice about the supplies that are being used, plan appropriately during procedures and avoid wastage.”
In this health care climate where budget constraints are in the forefront, Dr Ho expressed his hope that any cost savings be re-directed back into the Endoscopy Unit so that it can be used to improve patient care. Dr. Ho believes every department in the hospital, region and beyond should look at how they can reduce costs, save money and avoid wastage.
Although this was a resource and time intensive exercise, Dr Ho believes the effort was worth it because of the very positive and encouraging results.

Working towards a more diverse, equitable and inclusive workplace for all physicians
Read More Read LessVancouver General Hospital and the Vancouver Physician Staff Association are exploring the disproportionate number of men to women in medical leadership roles within VCH.
With support of VCH, they hired a facilitator to go through an Appreciative Inquiry process. Together the group of women and men, front line staff and senior leadership came up with an action plan.
Read full story and action plan here (originally published on the VPSA website) >

Reconnect with meaning and purpose: Tips from Dr. Stephen Swensen, Mayo Clinic
Read More Read LessTrusted expert and internationally recognized caregiver advocate for reducing clinician fatigue and improving employee engagement, Dr. Stephen Swensen, Professor Emeritus, Mayo Clinic, met with members of the Vancouver Physician Staff Association this January. He shared lessons learned over his three-decade-long career with the Mayo Clinic.
“Many physicians are working in a state of professional distress,” stated Dr. Swensen. “This goes beyond burnout and includes PTSD, emotional exhaustion, clinical depression, moral injury, compassion fatigue, and suicidal thoughts. When you’re in this state, you’re more likely to make a medical error. You have relationship problems, addiction problems; your productivity goes down as does your level of quality of care. One of the biggest opportunities we have to improve patient care is by caring for each other.”
An ideal workplace has three elements that Dr. Swensen calls agency, coherence and camaraderie. The happiest teams at the Mayo Clinic, he said, have the agency to make decisions, feel connected to their group, and celebrate each other’s milestones.
Leadership behaviours
Dr. Swensen identifies five behaviours (Leader Index Behaviours) that make for better leaders:
- They are inclusive.
- They communicate transparently.
- They value your ideas.
- They are interested in your career.
- They appreciate your work.
Mayo Clinic staff are surveyed annually on how their leaders rate in these areas. Those with low scores are coached to improve these or are moved out of leadership roles because leaders who don’t exhibit these five behaviours are causing harm to patients.
Medicine is a calling
Some people go to work every day for the paycheque; others see their career as a means to accomplish goals and receive acknowledgement of their contributions. It is common for those who choose a career in health care to also see their work as a calling, as a means of helping patients, their families and the greater community. When that sense of purpose is lost, said Dr. Swensen, physicians can develop professional distress.
“Engagement is the antipode to burnout; it connects us to meaning and purpose,” he said. “The number one driver of happiness is meaningful work so you would think health care should have the lowest rate of burnout. But sometimes we lose sight and have to be reconnected to our purpose. Coherence can do that. Coherence exists when all parts of the system fit together to form a united whole.”
To create coherence, leaders need to ask, listen and empower.
“It’s that annoying pebble in your shoe that holds you back rather than the mountain you need to climb. The research is clear that when departments work together to identify the ‘pebble’ they reduce burnout. You can apply this to Cerner. Superusers could monitor who’s using the system on weeknights and weekends and then ask them if they need assistance. A superuser can save a physician three to five hours a day by teaching them shortcuts.”
Architects rather than carpenters
The pronouns we use when we talk about our organization are a clue to how well that organization is thriving. When we think in terms of ‘us’ and ‘them’ rather than ‘we’ and ‘our,’ the institution flounders.
“If physicians are treated as partners, they behave that way,” said Dr. Swensen, who recalled how the Mayo’s chair of haematology addressed her team’s high burnout rate.
“She decided to be a leader, a champion—rather than a middle manager. Instead of saying this is what they’re telling us to do, let’s all just be carpenters, she empowered her physicians to be architects. They weren’t going to be told how to do something by people who don’t understand what they do. The team created the solutions.”
When we do our work, improve our work, and care for each other, our patients have the best doctors imaginable. Lean into tomorrow, Dr. Swensen encouraged, to see what difference you can make.
Further reading: Finding and Creating Joy in Work white paper (IHI white paper, co-authored by Dr. Swensen)
Article and photos submitted by the Vancouver Physician Staff Association (VPSA) >

Technology Innovation Engagement Forum brings physicians together
Read More Read LessCreating a Community of Innovation
Dr. Doug Courtemanche demonstrates an innovative tool for trainees, teachers and programs
More than 150 physicians, healthcare leaders and industry partners attended the first-ever Technology Innovation Engagement Forum held January 25 at VGH. The event provided an opportunity for physician innovators to share their insight and experience and make connections to support the development of innovative technology solutions for health care.
“This event is about bringing people together to start the conversation about the role of technology in healthcare,” said Dr. Kendall Ho, who co-chairs eFIT (engagement For Innovative Technologies) with Drs. Eric Cadesky and David Wilton. This is just the beginning.”
Innovative ideas in action
Dr. Corinne Hohl, VGH emergency physician highlighted a software application for reducing repeat adverse drug events, Dr. Jan Venter, family physician, shared a “check-engine light” concept to monitor brain vital signs such as in concussions, and Dr. Igor Brodkin, VA Anesthesia compared the OR activity whiteboard to airline industry technology, which inspired the creation of an OR real-time Activity Display Board. These were among the many ideas shared throughout the evening.
The event, sponsored by the VPSA Facility Engagement Initiative, VGH & UBC Hospital Foundation and supported by Vancouver Coastal Health, was also livestreamed via webcast. Tweets were flying as presentations sparked ideas and generated interest. There are already requests to hold another forum again soon.

Looking after physician health at Vancouver General Hospital
Read More Read LessMost physicians would agree there are not enough hours in the day to fit everything in. Patients are the priority, which means “luxuries” like exercising and socializing often get pushed aside. As a result, many physicians are isolated from their colleagues and neglectful of their own fitness and health needs. A new program, funded through the Vancouver Physician Staff Association (VPSA) Facility Engagement Initiative brings physicians together – for fitness and for conversation.
Physician-only spin classes are offered in the Centre for Cardiovascular Excellence at UBC Hospital. Classes are free and available every Tuesday at 6:30 am and every Thursday at 6:00 pm.
A personalized approach:
Physicians create a profile, which they will log into at the beginning of each class when they select a stationary bike. Progress is tracked and physicians are provided with objective measures of their fitness after each class so they can compare results and monitor improvement over time. Physicians also have the opportunity to participate in a monitored telemetry session providing continuous ECG.
A healthy breakfast is served after each morning class, providing time to connect before getting on with the day. VPSA funding supports the trainers, cardiovascular technicians and pays for breakfast.
“So many physicians are feeling burnt out and disconnected, this class gets the endorphins flowing and helps strengthen relationships among physicians and across disciplines,” explained Dr. Saul Isserow, Physician Project Lead for this initiative. “When physicians look after themselves they are in a better position to look after their patients.”

Collaborative, coordinated effort improves ED flow & capacity at Lion's Gate
Read More Read LessDr. Kristian Hecht, a Emergency Department (ED) physician at Lions Gate Hospital (LGH), thought there was a better way to leverage the floorplan and manpower available to the Emergency Department (ED). She had watched as ED patient volumes increased steadily each year over the past seven years – often the patient volume exceeded the ED capacity. Out of necessity, the waiting room sometimes became the treatment/assessment space.
The Lions Gate Hospital Physician Society as part of the Facility Engagement Initiative supported Dr. Hecht in pursuing this work.
Dr. Hecht saw that the First Aid area with its 19 patient care spaces could be transformed to manage and assess ambulatory patients and the RAZ area changed into the First Aid space. In addition, the ED wanted to adopt a patient assessment/treatment process developed at a Calgary ED.
This two-pronged approach was proposed and involved collaboration and coordination with ED stakeholders (MD, RN, EHS, RT, DI, portering, stocking, lab and ECG), LGH acute care administration and LGH project management office.
Triaging to new zones allowed both spaces to be used adequately and sharing the workspace between MDs and RNs far improved communication. The patient assessment/treatment process better organized the waiting room and enhanced patient safety. Recliner-style treatment chairs provided more effective use of space, while maintaining patient comfort and privacy. Touchdown assessment rooms prevented patients from blocking care spaces and allowed ample space for assessments/consultations. As well, re-directing patient flow reduced redundant tasks.
The result is improved patient flow through the ED, reduced patient wait times, improved communication between MDs and RNs, decrease in non-physician tasks, improved patient safety and satisfaction, and improved organization and scalability for future demands.

Record physician turnout for disaster preparedness at VGH
Read More Read LessA record physician turnout for a Disaster Preparedness Day for Vancouver General Hospital was made possible through the Vancouver Physician Staff Association (VPSA) Facility Engagement Initiative. Eleven physicians were able to participate in the event, along with two Vancouver General Hospital (VGH) emergency physicians and a trauma surgeon who helped to coordinate the day.
In total, more than 60 participants took part in the all-day event which was designed to test VGH's capacity to respond in a disaster situation, and was led by Susan Harris-Salt, Nurse Educator, ED and a team of VGH emergency nurses.
"The day was a success from a physician engagement perspective and as a disaster preparedness event," said Dr. Chris Lee, one of the two emergency physician leaders. "Having this many physicians participate is a great improvement from our last event."
Staff rely on established protocols and processes to guide them during a disaster situation. These were put to the test during the Education Day as the group launched into a table-top exercise with role playing providing valuable insight into what works, what needs to improve and how people are likely to respond.
In addition to testing protocols and processes, participants rotated through skills development stations including needle chest decompression, tourniquet application and radio readiness. Representatives from the Canadian Armed Forces and Canadian Blood Services also participated.
The event identified opportunities for improvement, including the involvement of more key stakeholders, such as ICU and radiology. Organizers were pleased with the results and the lessons learned. The success of the day was due in part to the many physicians who took part. An ongoing process, the next exercise will lead up to a full-scale, city-wide exercise to be held in spring 2018.


Specialist Services Committee © Doctors of BC









