- Fraser Health

Maternity service wait-times drop from 3 months to 3 days
Read More Read LessDr Charlene Lui, a family physician at the Burnaby Maternity Clinic, led a project to reduce clinic referral wait-times from up to 90 days to just a few days through an SSC Physician Quality Improvement. Read the story here>

Surrey Memorial Hospital to start emergency physician residency program
Read More Read Less- Dr. Sally Barrio, an emergency physician, has helped champion new ER physician training at the Surrey Hospital, reportedly the busiest ER in Canada with over 450 patients a day. It has been a dream for a some time at Surrey Memorial. READ MORE >

Burnaby Hospital Engagement Efforts Pay Off
Read More Read LessBurnaby Hospital physicians have been working to leverage the Facility Engagement opportunity to improve patient care and their workplace, and to build relationships among physicians and with the hospital administration. Their efforts are paying off. The following are a few examples of the great work underway that is leading to positive changes for the hospital.
Education Forum: Community Physicians Meet Specialist Services
Project Lead: Dr. Chris Bozek
Burnaby community physicians had little information about the existing speciality services and resources that Burnaby Hospital is able to provide to their patients. Furthermore, some physicians expressed lack of awareness about how to successfully refer their patients to the speciality clinics such as the orthopedics or neurology clinics at Burnaby Hospital.
So they set out to increase the knowledge and awareness of the hospital's specialty services, and establish effective communication between all physicians to improve patients’ experience in receiving timely and appropriate care. Their goal was to ensure patients have access to the right treatment to the right patient at the right time - every time.
Changes made: A steering committee was formed with the Burnaby Hospital project champion and Executive Director, and the Division of Family Practice, to discuss potential topics of discussion and best way(s) to present information. Three meetings were held, and a number of different topics were generated.
Project Outcomes: 3 education forum events have been held with over 30 participants attending:
May 3, 2018 – Ortho 101 - Review of the central intake for Orthopedics
- Overview of hip arthroscopy and minimally invasive hip replacement
-10 myths around Orthopedics
- Roundtable discussionOctober 18, 2018 – Neurology - Migranes/Headaches
- Multiple Sclerosis
- Seizures & Epilepsy
- Neuromuscular Disorders
- Roundtable discussion - Improving Access to Neurology Consults in BurnabyApril 10, 2019 – Chronic Pain Management - Procedures for pain management
- Medical management of chronic pain
- Pain management programs
- Roundtable discussion – Future initiatives on pain management wants and needsParticipant feedback was collected for each of the education forums. The feedback was positive with physicians requesting additional events to be held. Burnaby family physicians feel that this is a great forum to interact with Specialists and allow for feedback on hospital programs. It also provides an excellent forum for Burnaby Hospital specialists to promote the specialised services available to patients in the community.
Reducing Inpatient Echocardiograms
Project Champion: Dr. Sarah Ostler
An echocardiogram (Echo) provides information about a patient’s cardiac condition. This test is available to both inpatients and outpatients at Burnaby Hospital. Many inpatients remain admitted in the hospital waiting for their Echo test, unnecessarily extending their inpatient length of stay. About 43% of the echocardiograms performed at Burnaby Hospital are ordered for inpatients. In 2017, approximately 51% of these inpatients remained admitted an average of 5 days longer than their expected length of stay (ELOS); where some of them could have alternatively received their test as outpatients.
Having patients wait for tests as an inpatient slows down the flow of patients’ discharge, reduces the hospital’s bed capacity, puts pressure on staffing, and unnecessarily challenges the hospital’s resources and their optimal operational allocation.
To solve the issue, a team of four physicians set a goal to reduce number of patients receiving inpatient echocardiograms. They trialed a new requisition form to test its effectiveness. Feedback was sought from the physicians and booking clerks to identify opportunities to improve on both the “document” and the “booking" processes. The trial was then repeated with a larger group of physicians in specific departments, then spread throughout the entire hospital.
Changes Made
- Site-specific echocardiogram booking requisition form created
- Education to support improved patient identification for outpatient booking
- Adoption of an electronic booking process:
- Standardize the booking process
- Standardize the information provided to appropriately book an Echo
- Reduce potential for errors in the system by spreading it across Fraser Health
The Project Team: Teamwork was critically important in carrying out a project of this scope and successfully implementing change. Having a multi-disciplinary team provided the right amount and level of expertise that was needed to move forward in decision-making and tackle challenges. The hospital administration was supportive and heavily involved in the project as it involved operational process changes, and the following resources/departments were included:
- Medical imaging
- PCCs
- Clinical form services
- Clinical policy office
- BUH Admin
- PQI
- Unit ClerksProject Outcomes: The project was a major success as By June 15, 2019, the number of patients receiving inpatient echocardiograms at Burnaby Hospital decreased by 15%. A project poster presented at the Physician Quality Improvement conference won 1st place.
Enhanced Recovery After Surgery (ERAS)Project Champions: Dr. Gavin Gracias & Dr. Katherine Hsu

The delay until full recovery after major abdominal surgery/rectal-pelvic surgery and radical cystectomy has been greatly improved by the introduction of a series of evidence-based treatments covering the entire perioperative period and formulated into a standardized protocol. Compared with traditional management, Enhanced Recovery After Surgery (ERAS) represents a fundamental shift in peri-operative care. The ERAS-care pathways reduce surgical stress, maintain postoperative physiological function, and enhance mobilisation after surgery. This has resulted in reduced rates of morbidity, faster recovery and shorter length of stay in hospital (LOSH) in case series from dedicated centres and in randomized trials.
Changes Made (ongoing)
1. PDSA checklist on charts to collect data
2. Patient education post op – providing booklets/questionnaire
3. Implementation of ERAS protocols i.e carb drink and warming blanketThe Project Team: The ERAS project is a Fraser Health initiative. Facility Engagement funding enabled physician champions to develop a strategy to implement ERAS at Burnaby Hospital, to liaise with local nursing and administration to facilitate implementation of ERAS, and to oversee implementation. Monthly meetings have been held with physicians, hospital administration, and nurses.
Project Outcomes: The project is ongoing and has been successful in implementation of ERAS protocols. As this is a Fraser Health initiative, having physician involvement has been key in moving the project forward. The next steps include collecting data to determine its impact.
Crucial Conversations: Skills to Deal with Daily Challenges
Project Champion: Dr. Paul Johar

The Crucial Conversations course helps people master the skills needed to candidly and respectfully handle high-stakes conversations, achieve better results and enhance relationships. At Burnaby Hospital, 35 physicians and 5 administrative staff members attended this 2-day course. Both worked together to improve skills needed to engage others when addressing challenging issues. They learned to recognize when a conversation becomes crucial and received tools they could use to deal with daily challenges.
This course was originally offered in 2017 with 40 Physicians attending, and due to its popularity was brought back in 2019. As a result of the 2017 course, a crucial conversations club was started at Burnaby Hospital. This club enables physicians to identify challenges facing physician leaders and utilize the skills learned in the course to deal with them.
Project Outcomes: 40 learners participated in the course with 35 registering in the learning management system and 21 providing feedback regarding their experience. The course was well received by learners with 95% of respondents saying they were satisfaction rate with the course, that is was a worthwhile investment of their time and that they would recommend to a colleague.
Participants enjoyed the practical learnings in the course and enjoyed learning from knowledgeable and experienced faculty. They are ready to go back and apply the skills in the workplace by preparing for the difficult conversations and focussing on an outcome that is mutually acceptable to all parties. Learners expressed interest in future training regarding engaging others, managing people effectively and leading change.
- Interior Health

Patient Simulation Expands at Kootenay Boundary
Read More Read LessPhoto credit: UBC Faculty of Medicine, Okanagan Campus
Facility Engagement is supporting medical staff from several departments at the Kootenay Boundary Regional Hospital in Trail to participate in the development of a simulation curriculum for different staff groups. One physician will work on ER based simulations, another will provide simulations for OR teams, and another will focus on providing "just in time," clinically-based simulations for critical care teams. After developing the curriculum, the physician lead for each area will also learn how to run the simulator, and provide educational sessions. The work will support local physicians and improve patient care.
-------------------
A perfect storm for patient simulation is generating new education and training opportunities at Kootenay Boundary Regional Hospital (KBRH) in Trail. As the acute care facility for Interior Health (IH) in the West Kootenay and Boundary region, the hospital supports a rural population of approximately 75,000 people. KBRH also serves as a primary learning environment for students with the Southern Medical Program (SMP) and resident physicians with UBC’s Kootenay Boundary family practice site.Dr. Scot Mountain, Director of the Intensive Care Unit, is one of the local physicians working closely with IH to develop a dedicated patient simulation centre for health professionals and learners.- Island Health

Preventing preterm births: physician-led initiative expands, save lives
Read More Read LessAn initiative created by two physicians on Vancouver Island is supporting maternity care providers to identify at-risk patients and use medical interventions to prevent preterm births. It can save lives and prevent devastating infant health issues, while helping families avoid the distress of travel to larger cities to access neonatal care.
Preterm births are the leading cause of perinatal mortality and morbidity in Canada and worldwide. Babies born before 37 weeks of gestation are at increased risk of severe and ongoing medical problems.Having a preterm baby is also stressful for parents, particularly those who live in smaller communities. Without access to specialized neo-natal intensive care, parents need to take time away from other children and jobs to seek care in bigger
 centres.
centres.Dr Jennifer Kask, a family physician attached to the Campbell River Maternity Clinic was aware of very high preterm birth rates in communities across Vancouver Island. Pre-term birth rates were as high as 25% among patients in 2016/17, compared to 7.4% and 7.8% in BC and Canada respectively (2013).
With the support of Facility Engagement funding, Dr Kask and Obstetrical specialist Dr Kirsten Duckitt set out to engage family physicians, midwives, and allied health providers in discussions about preventing pre-term births.
Simple intervention identified
They found that a simple vaginal progesterone intervention that helps at-risk patients extend their pregnancy to bring them closer to term was often used in specialist care by obstetricians, but not always by other providers or patients.
"We concluded there was a gap was in the knowledge of our colleagues and patients," says Dr Kask.
"We also knew a main risk factor for a mother having a preterm birth is having had a preterm birth previously," Dr Kask says. "So it was a matter of how we help to educate our colleagues and provide some resources to identify who is at risk, and how to help prevent recurrent preterm birth."
Creation of a pathway and resources for providers
Those insights led to their development of a Preterm Birth Pathway and education to help providers identify patients at risk, and use evidence-based, effective medical interventions to prevent preterm births. They created a package of resources including:
- a case-based CME event
- a care algorithm
- a clinician resource (a pre-printed Special Authority form developed through discussion with Pharmacare)
- patient education materials that included patient cards and posters
With education sessions and provider adoption underway in communities around Campbell River, Dr Kask then accessed SSC Spreading Quality Improvement Initiative funding expand the work more widely across Vancouver Island, including to Port Alberni and Tofino.
They also spread the education through the Cowichan Valley through direct work with the Cowichan Tribes. Dr. Kask notes that preterm births disproportionally affect First Nations individuals and created education resources to support those communities.
Results and next steps
Through data collected in her maternity clinic, Dr Kask notes there has been real progress in preventing preterm births, both through measurement in her clinic showing a downward trend in pre-term births, and patient experience stories.
Dr Kask and Duckitt continue to spread the work across Vancouver Island rural communities through 2023/24. She then hopes to further spread it across all BC regions, where providers and patients in smaller communities share the same experiences and risks, and can benefit from the pathway and interventions identified.
Dr Kask says that one of the highlights of the project has been making specialized care more accessible to other providers. “The neat part of it has really been the relationship and mentorship I’ve received from my colleague Dr Duckitt. She is an excellent educator, a wonderful OBGYN and was so willing to share her specialist knowledge.”
“When a patient delivers at term in their own community, and says, 'I am so grateful that I didn't have to go to an NICU this time.' it warms my heart. Particularly because it implies that they have a little person at home."
"I recognize that we are not going to able to prevent all preterm births, but recognizing that preterm birth is the biggest cause of perinatal morbidity and mortality, aren't all of them worth trying to prevent?" – Dr Jennier Kask
- PROVIDER RESOURCES: Pathway and patient posters
- WATCH: From Idea to Action to Spread: Dr. Jennifer Kask
- WATCH: Dr. Jennifer Kask: Raising Awareness on World Prematurity Day
This project has been funded by the Specialist Services Committee Facility Engagement and Spreading Quality Improvement initiatives. The Specialist Services Committee is one of four joint collaborative committees representing a partnership of Doctors of BC and the Government of BC.

Physicians Lead the Way to Hospital at Home
Read More Read LessVictoria-area physicians have engaged providers and partners from across the hospital, region, and at government levels to introduce a new model of care for Hospital at Home to BC.
Victoria Hospitalists Dr. Elisabeth Crisci and Dr. Shauna Tierney have been unwavering in their pursuit of a new kind of care for patients. Now, their passion project is about to become a reality with the BC Government’s launch of Hospital at Home across the province.
With Hospital at Home (HaH), acutely ill adult patients who are at lower risk and have a predictable clinical path can get hospital-level care from a team of professionals at home, safely and effectively. The model has been used for years in countries like Australia and the UK.
Extensive studies, including three Cochrane reviews (Ref 1), show that HaH provides equivalent or better clinical outcomes than standard hospitalization. Length of stay tends to be shorter and there is a higher level of satisfaction amongst patients, their caregivers and healthcare workers. It also shields patients from some of the complications associated with a brick and mortar hospital stay.
Dr. Crisci first saw HaH in action several years ago while doing fellowship training in Australia. “This was not home and community care. It was acute, hospital-level care: IV medications, blood transfusions, oxygen. There is no doubt in my mind that those patients, if they were back in Canada, would need to be on a hospital ward.”
“A hospital is an unsettling environment, especially for frail and elderly patients,” she says. “I thought, ‘why can’t we do the same in Canada?’ The expertise and therapies that we associate with hospital care are all portable, and so is the hospital staff.”
“It is an opportunity to offer safer, more patient-centered care for our patients and for less cost. It is the right thing to do.”
Back in Canada, she often thought about the HaH model. Then, in 2019, an opportunity came up to take action. Her Hospitalist colleague, Dr. Shauna Tierney, was reading about a HaH program for COPD and was inspired.
“I saw that we could do better for our patients’ dignity and comfort, and thought, “we have a moral imperative to do this." - Dr. Shauna Tierney
Dr. Tierney reached out to Island Health and her Hospitalist colleagues to see what could be done. Dr. Crisci was ready. “We knew that we needed to join forces to make this happen.”

Left: Dr Elisabeth Crisci. Right: Dr Shauna Tierney
Collaboration moves the vision forward
The two physicians would need help to develop a HaH program for BC– including the buy-in and support of the Island Health, South Island Hospitalists, the Divisions of Family Practice, and eventually, the Ministry of Health. Funding from Health System Redesign and Facility Engagement made that possible.
“Over the past year we worked relentlessly to get the level of engagement this project requires, while developing our own HaH program for B.C.” says Dr. Tierney. It meant that they had to become agents of change, inspire others to think outside of the box, and challenge some old-standing beliefs about how hospital-care can be delivered.
“The same old thinking will always give you the same old results,” says Dr. Crisci. “We argue that what should define hospital-level or acute-care is the type of patient and the type of clinical interventions required, rather that adhering to a definition based on the physical location of the patient.”
Taking the hospital team and interventions to the patient's home would require further support, which they sought from the BC Ministry of Health. “We don’t want this to be just another community-based service,” says Dr. Crisci.
“We want a true substitute to a standard hospital admission. For this to be possible, we have to ensure that these patients fall under the governance of the provincial Hospital Act. This means that even if at home, these patients are admitted and under the responsibility of the hospital.”
To their delight, the Ministry was interested in doing much more with HaH, and in September 2020, announced that BC would introduce the model to Victoria, and then spread it across the province. In part, HaH can help with the government’s COVID-19 planning by freeing up some acute care capacity.
Next steps
While there are details to iron out to pilot HaH at Victoria General Hospital and eventually scale to other hospitals, a full-time project team is in place to take the work over the finish line. The doctors are continuing as medical leads.
They note that experienced physicians on the ground are uniquely positioned to bring innovative ideas such as this to the fore. But they could not have done it alone. It took everyone’s help to make their vision a reality.
“It has been quite an adventure. It started with two physicians with an idea, and now HaH is one of the priorities for BC’s health care system,” says Dr. Tierney.
“The collaborative effort between the Ministry, Island Health and the front-line physicians has been incredible; something I never thought I’d ever witness in my career,” agrees Dr. Crisci. “Here we are, side-by-side, to not only improve the care of patients but also working to make our system a bit more sustainable.”
"I can’t wait to see that first patient’s face when I can say, “you get to go home, and I will come to see you at home.” - Dr. Elisabeth Crisci
Funding for physician engagement in the HaH project was provided by Health System Redesign (HSR), an initiative of the Joint Collaborative Committees (JCCs) representing a partnership of Doctors of BC and the Government of BC – and the South Island Medical Staff Association, funded through the South Island Facility Engagement Society and Specialist Services Committee, one of the four Joint Collaborative Committees.Ref 1: Cochrane Reviews
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD007491.pub2/full
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000356.pub4/full

Comox/Campbell River: Facility Engagement Changed Everything
Read More Read Less~~When the Campbell River and Comox Valley Hospitals (one-hospital, two campuses) opened last October, the transition from the old St. Josephs’ Hospital was welcome, but rocky. The design of the new spaces were not as workable as expected, and patient flow and congestion challenges in the ER escalated within the first few weeks. Around the same time, patient visits increased significantly. “Within the first few weeks, the entire back half of the emergency room was filled up with admitted patients,” says Dr Albert Houlgrave, Emergency Room Physician and lead on this Quality Improvement project.
He explains that physicians and frontline staff were feeling stressed about the congestion and patient safety, but did not feel their concerns were being heard by health authority administrators who were not in the hospital every day. So they met on their own time to brainstorm solutions - a process that created good ideas, but also created some friction with the health authority counterparts, who were not involved in the discussions.
That’s when Facility Engagement came along, and the Physician Engagement Society of Courtney & Comox Initiative (PESCCI) was formed. The groups began to talk. Facility Engagement created a platform for dialogue between physicians and administrators to look at their common goals. “Facility Engagement funding relieved some of that pressure to be regularly volunteering our time and energy when so many of us were already extremely busy”, he says “And it created a culture where we could meet to discuss solutions to the problem and subsequently meet with administration to put those ideas into action.”
Once meetings started, improvements happened quickly: a dedicated trauma bay, a hot stroke protocol, simulation training, redeployed nursing support for waiting patients, improved hospital signage, a new paging system and space redesign for new beds. “It was great to have administration on our side to help free up space and make new space for beds.”
Physicians, nurses and unit clerks also began to review patient cases to find further improvements to flow and efficiency, and with administration, were able to put their ideas into action.
“While we have been working hard within the ER to improve the frontline work, we have also been reaching out to other departments.” said Dr Jennifer Laurence, the co-lead physician on this project, adding, “To date we have had the Laboratory Department, Maternal/Child, ICU, and the Medical/Surgical Unit invited to our quality meetings to review issues of concern regarding patient care and ongoing relationship building between our departments.”
Today, the situation has turned around completely. Communication and teamwork between physicians and administrators has grown, and the culture has evolved. “We have more time to give, and have been supported by PESSCI under the umbrella of quality improvement, flow and efficiency,” says, Dr. Houlgrave. “From there, it has blossomed into a multitude of mini-projects and ideas.”
Dustin Spratt , Manager Emergency & Critical Care, ICU for Campbell River and Comox Valley Hospitals notes that administrators and physicians are enjoying a good working relationship, close communication and regular meetings, and are now looking at collaborating across the two sites. “The importance of Facility Engagement is critical in providing good quality patient care,” he says. “We have front line clinical and administrative operational levels of responsibilities. And to make it function well, we need to have good communication and relationships. Through collaboration we’ve been very successful with managing the change, and have been able to put a lot of quality improvement into play. Everyone is now collaborating around quality goals and successfully managing important changes.”
- Provincial Health Services Authority
Pandemic validates engagement process for system improvements
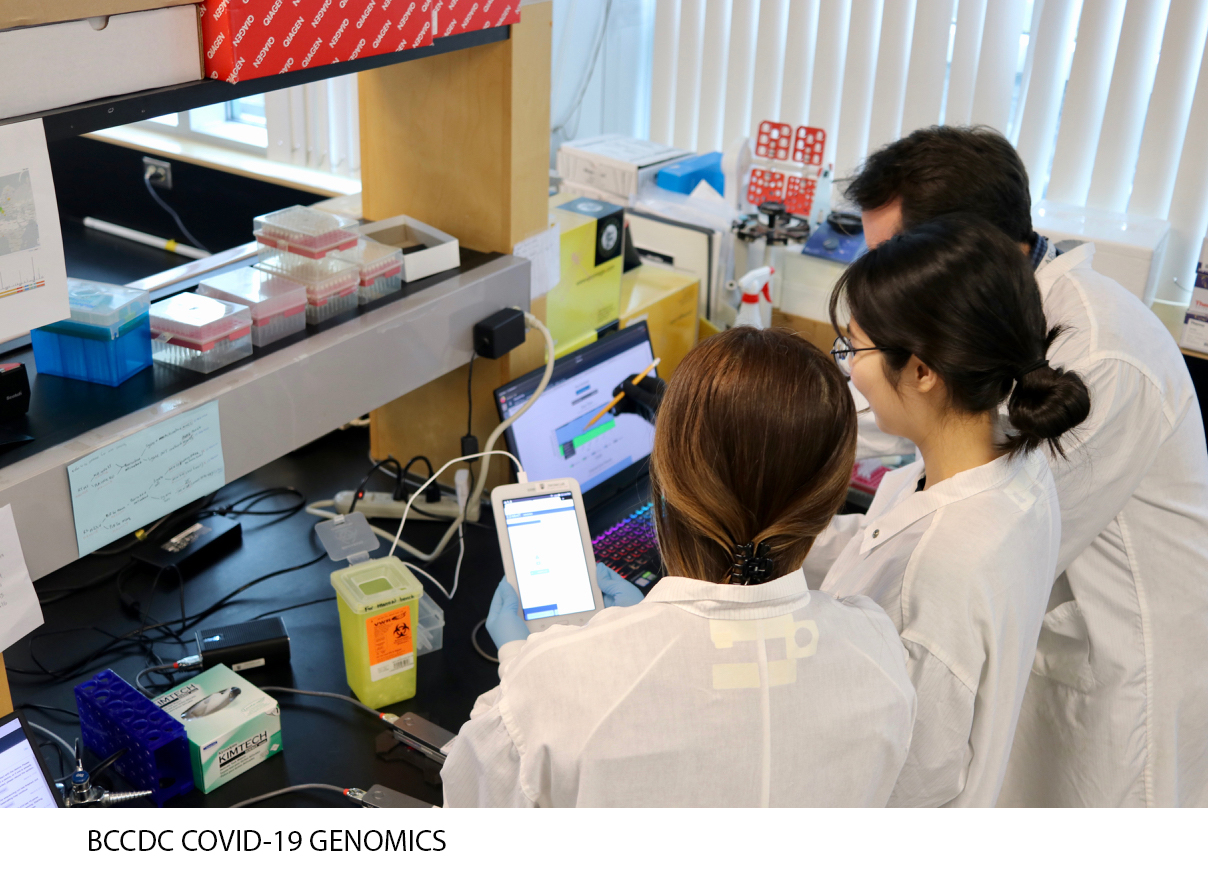
Read More Read LessBCCDC Public Health Lab Client Engagement Feedback Project

In 2019, the BC Centre for Disease Control Public Health Laboratory (BCCDC PHL) set out to solicit stakeholder satisfaction feedback about current BCCDC PHL service delivery, with an eye to inform future service improvements.
As the province’s primary public health testing facility and microbiology reference lab for infectious diseases, the timing was fortuitous. COVID-19 would arrive on BC’s doorstep a few months later, shining a light on the laboratory’s essential role in enabling a coordinated provincial public health response to a global pandemic caused by an emerging pathogen.
Over the years, public health priorities and technologies had evolved, and the demand for PHL services had increased. Future modeling was needed to optimize services, turnaround times, operational and scientific capacity and resources, to effectively meet
the ongoing needs of the public, physicians and organizations across BC.
A pandemic was always on the radar as one of the laboratory’s many areas of focus. “Preparedness for a pandemic is one of the key priorities of a public health lab,” noted Dr Linda Hoang, Medical Microbiologist and Associate Medical Director and Program Head. “We were concerned about surge capacity and we wanted to find more efficient ways to streamline services.”
The PHL would need to tap into a wide variety of insights from BC physicians and organizations served by the laboratory to fully understand all of its strengths and opportunities for improvement.
So Dr Hoang – along with project co-leads, Dr Mel Krajden, Medical Director, BCCDC Public Health Laboratory and Karen Mooder, Director, Laboratory Operations – set in motion a BC-wide consultative process to identify PHL service expectations, gaps and challenges, and to seek potential solutions and recommendations from the clients themselves.
Engagement of this scale across a massive community of practice was no small undertaking, and Facility Engagement funding was key to enabling nimble deployment of resources to support realization of project outcomes.
The first step was to secure leadership for the project from Dr Perry Kendall, Clinical Professor at the School of Population and Public Health, and BC’s former Provincial Health Officer. Respected by administrators and physicians, Dr. Kendall is well-versed on the wide range of topics of interest across the public health landscape.
To support Dr. Kendall in facilitating dialogue across a diverse stakeholder group served by BCCDC PHL, a consultative framework was designed. Both clinically and operationally driven, it entailed dozens of one-on-one interviews and planning meetings that spanned five geographic health authorities, the Provincial Health Services Authority, and First Nations Health Authority (FNHA) and included:
- Public Health Managers
- Medical and Clinical Microbiology Team members
- BC Medical Health Officers
- 22 Physician participants including:
- General Practitioners
- Medical Microbiologists
- Infectious Disease physicians
- Physician Epidemiologists
- FNHA physicians
These consultation sessions also included senior operational and medical leads to provide appropriate clinical and operational context. All partners worked hand in hand with each other every step of the way, from project planning, to interview design, to communications.
“It was a true engagement effort, top to bottom,” said Jennifer Diep, Project Manager for BCCDC Facility Engagement. “Administrators and physicians always had an opportunity to provide feedback on an equal basis. It was very empowering.”
“It was everyone’s project – an operations project as much as a physicians’ project. That really improved connections, trust, and collaboration.” - Jennifer Diep
Further, when Dr Perry Kendall presented findings in a report, additional stakeholders were engaged, including scientists, public health students, laboratory trainees and administrators.

What did those findings show? Overall, a high level of satisfaction with the PHL service, including reference lab functions, expertise in interpretation of results, outbreak management support, and development of appropriate diagnostics. Concerns were also heard about the limited level of investment and lack of surge capacity at the time, and the need for a provincial strategy for diagnostic services and investments in future diagnostic and surveillance technologies, including genomics.
Many solid, specific recommendations were put forward for a future plan. But then, COVID-19 came along.
While there was no time to act on the report’s findings, the value of the engagement process was fully validated, as both the strengths and limitations heard from stakeholders were tested during the outbreak.
“The findings really showed up in this pandemic,” said Dr Hoang. “While we did not have the capacity and resources initially to get up to speed as quickly as we would have liked, our requests for resources were quickly supported, which allowed us to ramp up successfully. We had to re-organise our operational workflow very quickly, but we knew what was needed and thankfully, we were supported to do our job."
When the pandemic settles down, it is expected that PHL’s future planning will proceed, informed by the engagement process, as well as some new, real-life insights.
Dr Hoang noted that the COVID experience highlights some of the concerns about the limitations of the health care system that have been raised by those on the front line, further emphasizing the importance of continued collaboration between physicians and health authorities in health care planning.
“The system needs to trust in our expertise. By expanding these kinds of engagement opportunities, physicians will have an organized way to alert the health care system of deficiencies and red flags to improve patient and population care.” - Dr Linda Hoang

- Core Laboratory Functions
- Diagnostic services
- Communicable disease surveillance, prevention and control
- Outbreak and emergency response to communicable diseases
- Environmental health, drinking water and food safety
- Reference microbiology testing, specialized screening/surveillance, and diagnostic testing
- Biosafety, bio‐hazard containment and response
- Integrated communicable disease data management
- Public health policy development and evaluation
- Laboratory improvement and regulation (quality assurance)
- Training and education of healthcare and public health workers
- Public health related innovation, applied public health research and development
- Vancouver Coastal Health

Working to advance Indigenous cultural safety at Vancouver Acute and Community sites
Read More Read LessVANCOUVER ACUTE AND COMMUNITY: It’s well known that our province’s Indigenous peoples have worse health outcomes than our non-Indigenous citizens. The systemic racism that exists in our health-care system and in both acute and community settings has been part of the background to the UN Declaration on the Rights of Indigenous Peoples, the provincial bill to implement UNDRIP, and the In Plain Sight report.
 We need to increase cultural safety for Indigenous patients and family members in both acute and community care. How to do this is the mandate of the newly formed Vancouver Physician Staff Association (VPSA) Engaging Physicians in Indigenous Cultural Safety (EPIC) Task Group.
We need to increase cultural safety for Indigenous patients and family members in both acute and community care. How to do this is the mandate of the newly formed Vancouver Physician Staff Association (VPSA) Engaging Physicians in Indigenous Cultural Safety (EPIC) Task Group.Born from the iCON VCH Indigenous Health Rounds, the task group will prioritize and advance Indigenous cultural safety in health-care settings. It will be guided by meaningful partnerships with:
- VCH senior leadership and VCH Indigenous Health leadership
- VPSA physicians
- Indigenous Elders, Knowledge Keepers, physicians, patients, and communities
- First Nations Health Authority
- BC Ministry of Health
- UBC Digital Emergency Medicine Intercultural Online Health Network (iCON)
“The task group came about with collaboration between VCH Indigenous Health and iCON on Indigenous health rounds,” said Dr. Kendall Ho, an emergency physician and one of the task group founders. “VPSA helped fund these innovative meetings and we found over time growing interest from health-care professionals (physicians, nurses, and allied health staff). Close to 650 people registered for our last session, with 68 physicians attending. With that momentum, we worked with VPSA to establish the new task group.”
VPSA advocated for additional funding for the work the group will do. It has provided guidance and stewardship to ensure the task group’s goals align with the Facility Engagement Initiative’s mandate. VPSA also offers sessional funding for physicians attending task group meetings.
The outcomes from the iCON-VCH Indigenous Health Rounds have been impressive.
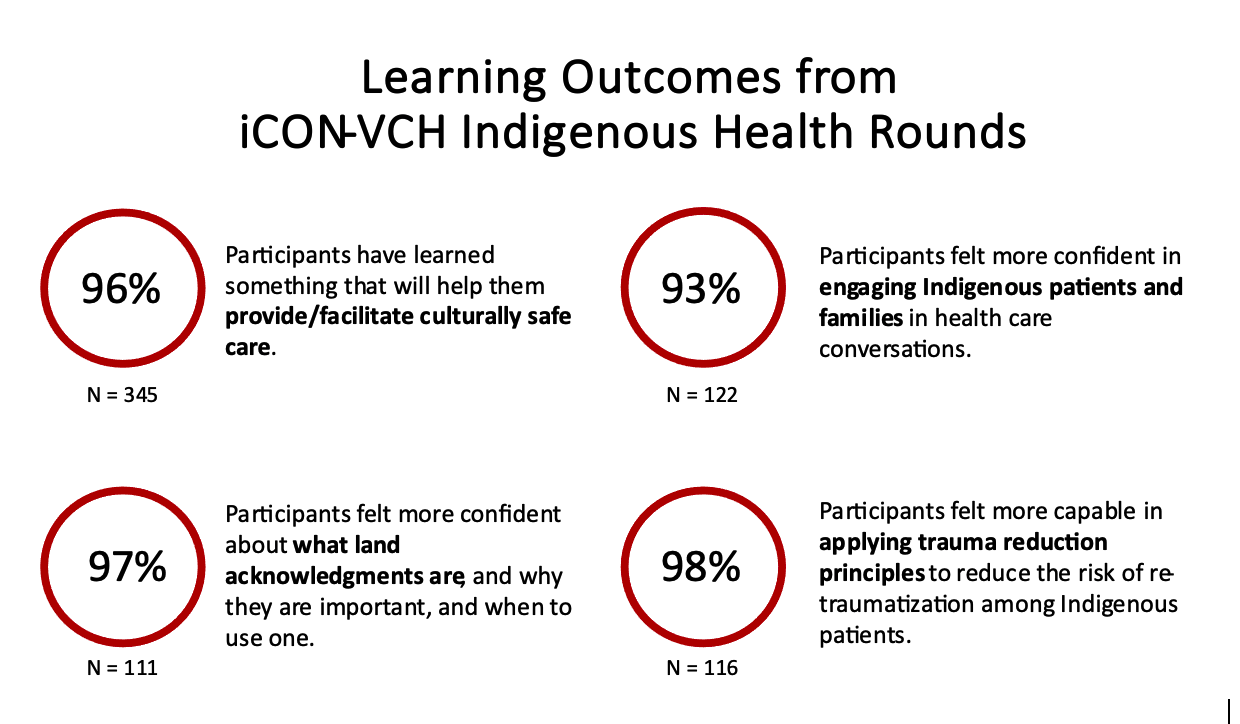
“Many of our physicians and health professional colleagues realize that even though we may not think we are racist, there is systemic racism and we, working in this system, sometimes display the behaviour of racism,” said Dr. Ho. “With that awareness, the majority of health-care professionals are interested in learning more to ensure all patients get optimal care.”
The EPIC Task Group has three key strategies for achieving its goals. These are continuing the iCON-VCH Indigenous health rounds, creating accredited educational resources, and developing a VCH Indigenous Health patient experience think tank.
VCH’s Vice President of Indigenous Health, Leslie Bonshor, is one of the executive sponsors of the EPIC Task Group. With her department, the task group is able to access and partner with Elders and Indigenous practitioners as well as engage with the First Nations Health Authority to make the health rounds good educational venues.
“Focusing on patients’ experience of care has to be a priority,” said Ms. Bonshor. “Physicians are used to questioning patients based on clinical experience, but we need to see a shift to understanding a patient’s experience of the health-care system as well in order to provide culturally safe care. This begins the moment an Indigenous patient walks through our doors.”
Ms. Bonshor and Dr. Ho are keen to share EPIC’s learnings with other health-care professionals across the province. Videos of previous Indigenous Health Rounds are available here, along with more information about them. Forthcoming educational resources will also be posted.
Dr. Ho’s hopes for the EPIC Task Group are high.
“I’d like to get to the point where Indigenous patients and caregivers feel free to come to us with no hesitation when they have health concerns, where they feel the health system is for them. It will be amazing when we get there.”
EPIC Task Group genesis
A chance encounter with an Indigenous patient visiting the VGH Emergency Department over 10 years ago set Dr. Kendall Ho on his “epic” journey.“The patient had been in a car accident, and I recommended X-rays for his neck,” recalled Dr. Ho. “He thanked me, but said he preferred traditional healing. It took me aback because I didn’t know what that meant. But it opened the opportunity for me to try to learn why he made that choice. It made me question my responsibility as a physician. I knew nothing about traditional healing, so as the hospital’s designated person in charge of this patient’s care, I felt incapable to decide if traditional healing was a suitable choice.”
Dr. Ho felt it was important to learn more. He was already working on the inter-Cultural On-line health Network (iCON) initiative and was in touch with Leslie Bonshor who was, at the time, the Indigenous senior leader in Fraser Health. He set off to help educate health-care professionals and himself to understand how we can approach and support our Indigenous patients better.
More than 10 years later, these initial steps led to the creation of VPSA’s EPIC Task Group.
Other ways VPSA is prioritizing cultural safety
Cultural safety for patients and health-care professionals is a top priority for VPSA. The association works closely with the VCH Medical Staff Diversity, Equity and Inclusion Steering Committee and several members sit on the committee and its three working groups. The committee’s purpose is to advance equity and inclusion for medical staff across the health authority and it achieves its mandate through a wide variety of activities.
Recent events that prioritize cultural safety include a presentation on creating a safe and inclusive space for transgender and two-spirit people by Dr. James Makokis and an Out Loud and Proud workshop during Pride Month on supporting 2SLGBTQIA+ people in clinical spaces.


Specialist Services Committee © Doctors of BC
